Hepatocellular carcinoma with macrovascular invasion treated with yttrium-90 radioembolization prior to transplantation
Introduction
Liver resection or liver transplantation (LT) is the therapeutic gold standards in patient with hepatocellular carcinoma (HCC) related with or without underline liver disease (1). Selective internal radiation therapy [yttrium-90 microspheres radioembolization (Y90-RE)] with yttrium-90 microspheres has been already successfully described as an alternative to transarterial chemoembolization (TACE) and ablation (2). Furthermore, Y90-RE was described has alternative downstaging for advance HCC (2). At our center, we are also increasingly using Y90-RE with yttrium-90 microspheres for the downstaging of patients with HCC beyond the Milan criteria for LT. We have applied this new strategy in four cases of HCC with portal vein tumor thrombosis (PVTT). According to the staging system of the Barcelona Clinic Liver Cancer (BCLC), patients were staged as BCLC-C. This paper comprises a presentation of the results following application of the procedure.
Methods
Patients
From January 2002 to day, 367 patients were transplanted at the San Camillo Hospital Center. Four patients were transplanted for HCC treated with Y90-RE before LT. All cases were discussed by a multidisciplinary panel of hepatologists, liver surgeons, interventional radiologists and anaesthetists. Inclusion and exclusion criteria of study were: (I) patient with a preserved liver function (serum bilirubin level <1.5 mg/dL, INR <1.3, and no signs of liver decompensation); (II) esophageal varices < grade 1, platelets count >80×109/L; (III) absence of ascites. Patients were considered eligible for Y90-RE if they meet all inclusion criteria. PVTT was defined with CT or MRI as a partially or complete occlusion of the vein, with enhancement of the thrombus in the arterial phase. An informed consent was obtained before the procedure for all patients. We analyzed in this study four patients with PVTT before Y90-RE.
Radioembolization procedure
The procedure was performed as previously described (3,4). In all cases a SIR-Spheres® Y-90 resin microspheres was used to perform the Y90-RE. The first patient had two treatments and the others three had one treatment. Median delivered dose was 1.9 giga Becquerel (Gbq) with range from 1.7 to 2.0. The first patient of our series was treated 2 times with a mean dose of 1.7 Gbq, the others three received one treated of 2.0, 1.9 and 2.0 Gbq respectively. Assessment of tumor response after Y90-RE was evaluated by the multidisciplinary staff according to the modified response evaluation criteria in solid tumors (mRECIST). At radiological follow-up, the PVI disappears in the four presented cases, therefore we re-discussed the cases and we included patients in the LT waiting list.
Results
Patients
Four patients with a PVTT were treated with Y90-RE prior to LT with an intent-to downstage the disease. Patients etiology were hepatitis C virus in all cases, one had an alcohol history, mean age at Y90-RE procedure was 57 and 58 years at LT. Means interval time between Y90-RE and LT was 15.86 months. Patients characteristics are resumed in Table 1. No death Y90-RE related or LT related was observed in this series. Before Y90-RE the PVTT was classified as Vp3 in one patient and as Vp1 in three patients. The four patients had a complete response for the thrombosis, enough to be included in the waiting list within the Milan criteria. MELD score at Y90-RE and at LT was not statistically different, but one patient was transplanted with a MELD score 24 after the 6 months of the Y90-RE due to a liver failure after the procedure. Patient had an increased bilirubin (7.4 mg/dL) and international normalized ratio (2.32) with ascites. Alphafeto-protein decrease significantly between Y90-RE treatment and LT in patient with high level of alphafeto-protein before Y90-RE, in the others three cases level was stable. Any of the patients receive adjuvant sorafenib after or before Y90 or before OLT. A preliminary results of 39.1 (range, 1–76) months of free-survival was obtained.
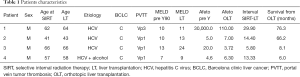
Full table
LT
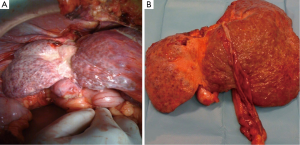
All livers were harvested from deceased after cardiac death donors. We had not particular surgical difficulties during LT procedure in those four patients comparing with the 18 cases without PVTT performed in our center. Surgical problems could be adhesions due to the Y90-RE treatment. In some cases we find a presence of tense fibrous tissue between the liver and diaphragm, or between the liver and inferior vena cava probably due to the resulting inflammation and edema. The hemiliver treated with Y90-RE appear hypotrophic with a contralateral hypertrophy (Figure 1). All patients were placed to immunosuppression regimen with everolimus.
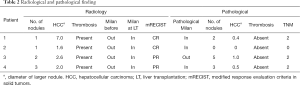
Radiological and pathological results
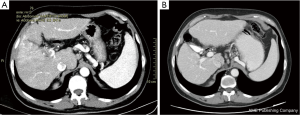
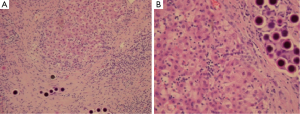
In two cases we had a complete radiological response according with the mRECIST classification, and in the last two cases a partial response was observed. In all four cases the complete thrombosis regression was observed (Figures 2,3). The pathological examination on the specimen of all patients find in one case absence of tumoral cells. In three cases the pathological exam was within the MC and in one cases was out but the larger tumor was 2 cm. No PVTT was observed, in one case a microvascular invasion was present. Pathological results are resumed in Table 2. In one case, a difference between the radiological and the pathological exam was observed. In these patients three nodules were not observed at the CT but observed at the macroscopic exam (nodule diameter was <5 mm).
Full table
Discussion
On this study, transplantation for HCC in BCLC stage C with macrovascular invasion after Y90-RE treatment has been successfully achieved. BCLC guidelines suggest that TACE is the standard of care in patients with intermediate-stage disease BCLC-B and in the other hand BCLC-C patients should be treated with palliative non operative therapy. However, HCC is a truly radiosensitive tumor with a predominantly arterial vascularization: for this reason, Y90-RE was developed with the aim of releasing a maximal effective dose just on the neoplastic tissue not influenced by the number, size or location of nodules, sparing the normal surrounding liver parenchyma. Y90-RE action is generally related to the radiation effect released on the tumor (5), while TACE is based on the ischemic effect. The release of Y90 on the HCC allows the treatment of patients who present a neoplastic macro-vascular invasion due to the high dose of radiations delivered on the hyper-perfused tumor, leading to an endothelial vascular injury (6). In our experience the mean time between the Y90-RE procedure and eventual LT should be 12 months at least (4). In one case LT was performed before this 12 months follow up after Y90-RE due to MELD increasing from 13 to 24 after 5.8 months of the Y90 procedure.
The heterogeneity of BCLC-B patients has been previously described and for this reason most recent papers have proposed to identify a subgroup of patients who could have a major benefit from Y90-RE instead of TACE (7). Moreover, Y90-RE begins to be proposed by different authors as a treatment of choice in patients with advanced BCLC-B and early BCLC-C (8). Furthermore other studies have shown that Y90-RE has a better response rate compared to TACE in patients with advanced BCLC stage (9). For this reason Y90-RE could be considered an effective tool for the downstaging strategy to LT in selected patients (10).
In this series we treat four patients with initial BCLC-C classification due to macrovascular invasion. In only one case the MELD increase after the treatment, the other three patients had no liver failure due to the procedure. Instead, in all cases a decrease of alphafeto-protein was observed. Furthermore, according with the mRECIST classification we had two complete responses and two partial responses. In all cases patients underwent to transplantation within the Milan criteria.
We obtain a free and an overall survival of 39.1 months without recurrence or death for these four patients. As shown by the group of Mazzaferro, our study confirms the efficacy of Y90-RE in patients with major macro-vascular invasion, consisting in a complete disappearance of the PVTT (10). We push the paradigm of these patients performing a LT.
Conclusions
We reported a short series of patients transplanted after Y90-RE in patients with BCLC stage C for PVTT. In our experience we achieved acceptable overall and disease-free survival. Eventually, Y90-RE seems to have a place in the downstaging strategy for LT candidates. Future study is needed to determine the role of Y90-RE as downstaging treatment.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by institutional ethics committee board of San Camillo Forlanini (No. 16/43), and written informed consent was obtained from all patients.
References
- Ettorre GM, Levi Sandri GB, Santoro R, et al. Laparoscopic liver resection for hepatocellular carcinoma in cirrhotic patients: single center experience of 90 cases. Hepatobiliary Surg Nutr 2015;4:320-4. [PubMed]
- Lewandowski RJ, Kulik LM, Riaz A, et al. A comparative analysis of transarterial downstaging for hepatocellular carcinoma: chemoembolization versus radioembolization. Am J Transplant 2009;9:1920-8. [Crossref] [PubMed]
- Strigari L, Sciuto R, Rea S, et al. Efficacy and toxicity related to treatment of hepatocellular carcinoma with 90Y-SIR spheres: radiobiologic considerations. J Nucl Med 2010;51:1377-85. [Crossref] [PubMed]
- Ettorre GM, Levi Sandri GB, Laurenzi A, et al. Yttrium-90 Radioembolization for Hepatocellular Carcinoma Prior to Liver Transplantation. World J Surg 2017;41:241-9. [Crossref] [PubMed]
- Sato K, Lewandowski RJ, Bui JT, et al. Treatment of unresectable primary and metastatic liver cancer with yttrium-90 microspheres (TheraSphere): assessment of hepatic arterial embolization. Cardiovasc Intervent Radiol 2006;29:522-9. [Crossref] [PubMed]
- Folkman J, Camphausen K. Cancer. What does radiotherapy do to endothelial cells? Science 2001;293:227-8. [Crossref] [PubMed]
- Bolondi L, Burroughs A, Dufour JF, et al. Heterogeneity of patients with intermediate (BCLC B) Hepatocellular Carcinoma: proposal for a subclassification to facilitate treatment decisions. Semin Liver Dis 2012;32:348-59. [PubMed]
- Salem R, Mazzaferro V, Sangro B. Yttrium 90 radioembolization for the treatment of hepatocellular carcinoma: biological lessons, current challenges, and clinical perspectives. Hepatology 2013;58:2188-97. [Crossref] [PubMed]
- Kulik LM, Atassi B, van Holsbeeck L, et al. Yttrium-90 microspheres (TheraSphere) treatment of unresectable hepatocellular carcinoma: downstaging to resection, RFA and bridge to transplantation. J Surg Oncol 2006;94:572-86. [Crossref] [PubMed]
- Mazzaferro V, Sposito C, Bhoori S, et al. Yttrium-90 radioembolization for intermediate-advanced hepatocellular carcinoma: a phase 2 study. Hepatology 2013;57:1826-37. [Crossref] [PubMed]


