Robotic assisted excision of type I choledochal cyst with Roux-en-y hepaticojejunostomy reconstruction
Introduction
Choledochal cyst is a relatively rare congenital disease which has a higher rate of prevalence in Asia (1). This disease is usually found in childhood, and approximately two-thirds of patients with this condition are found at pediatric age (2). However, the number of patients diagnosed with a choledochal cyst has increased in adults due to improved imaging modalities and increased health check-ups. It is also reported to be more common in young women, who may be more concerned in cosmetic result when surgery is to be carried out (2,3). Originally described by Vater in 1723 (4), choledochal cysts are now commonly classified using Todani modification of the Alonzo-Lej classification system (5). The type I choledochal cyst consists of cystic dilatation of entire common bile duct which maybe either cyst, saccular, or fusiform type and accounts for 85-90% of all cases (6,7). The current standard treatment of choice for choledochal cyst is complete excision with Roux-en-y hepaticojejunostomy due to possible associated complications if left untreated, such as cholangitis, pancreatitis, cirrhosis, portal hypertension, and biliary malignancy (3,8). Minimal invasive approach has gain wide interest in recent years, especially with the use of robotic surgical systems which can facilitate complex minimal access procedures (1,2,9,10). Herein, we present a case of robotic assisted excision of type I choledochal cyst in a young lady with complete intracorporeal reconstruction of Roux-en-y hepaticojejunostomy.
Case presentation
We present a video case of a 26-year-old female who presented to our hospital with symptoms of epigastric pain and radiating pain to back for several months. Physical examination was negative. Total bilirubin was 1.53 mg/dL (normal range: 0.2–1.6 mg/dL); alkaline phosphatase was 103 U/L (normal range: 10–100 U/L); gamma-glutamyl transferase was 220 U/L (normal range: 8–60 U/L); carcinoembryonic antigen was 0.8 ng/mL (normal range: <6 ng/mL); carbohydrate antigen 19–9 was 24.7 U/L (normal range: <34.6 U/mL). Magnetic resonance cholangiopancreatography revealed a large round cystic mass at porta hepatis region, 5.4 cm × 4.6 cm in size connecting to distal common bile duct and jointing to pancreatic duct. According to the Todani classification, it was the type I choledochal cyst. She underwent robotic assisted total excision of the choledochal cyst with Roux-en-y hepaticojejunostomy reconstruction.
Surgical technique
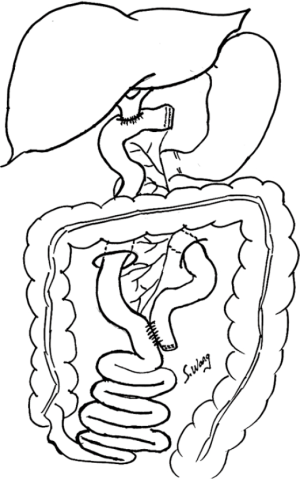
The procedure is reported on Figure 1 and summarized in Figure 2. The patient was put in reverse Trendelenburg position with the table tilted towards left side, so that right side was about 15–20 degrees up. Da Vinci Robotic Surgical System (Si model, Intuitive Surgery) for this procedure was used. Five ports (4 robotic trocars including 12-mm camera port, and 12-mm accessory port) were used for the excision of this type I choledochal cyst with roux-en-y hepaticojejunostomy reconstruction. Since this patient was a thin lady with a body mass index of 17 and a narrow costal margin, thus the design of the trocar ports needed to be more downwards. A transverse open method incision about 5 cm below the umbilicus was made for the 12-mm camera port, and pneumoperitoneum was developed with a pressure of <15 mmHg. Three 8-mm robotic working ports were placed; one was at anterior axillary line of the left side of the patient’s abdomen 2 cm below the subcostal margin, and the other two ports were placed on the right side, with one at the anterior axillary line just below the subcostal margin and the other at the midclavicular line between the camera port and the right side robotic port at the level of umbilicus. A 12-mm accessory port was placed in between the camera port and left side robotic working port about 2 cm below the umbilicus. After all the ports had been placed, the robotic system was docked into position.

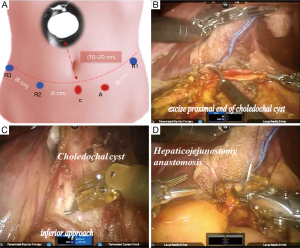
Cholecystectomy was performed first after ligating the cystic artery and cystic duct. The choledochal cyst was approached in four directions, inferiorly, medially, laterally and superiorly to dissect off its surrounding tissues. The choledochal cyst was dissected inferiorly all the way to the normal part of distal common bile duct and ligated with hemoclip and then transected. The superior part of the choledochal cyst was also dissected to identify the normal part of common hepatic duct. The choledochal cyst was resected completely, and reconstruction of hepaticojejunostomy was arranged. Roux-limb of the jejunum was prepared first, and hepaticojejunostomy was performed using 3-0 Vicryl with interrupted-suture fashion (Figure 3). End-to-side jejunojejunostomy was performed using autosuture stapler and the defect was closed.
This surgical procedure took 480 minutes to finish successfully. The total blood loss was 100 mL and no blood transfusion was needed. Postoperative recovery was complicated with Roux-limb obstruction causing bile leakage which was resolved by laparoscopic approach and percutaneous transhepatic cholangiography and drainage for diversion of bile. Thereafter, the patient recovered uneventfully and discharged home on postoperative 4th week.
Discussion
Before the era of minimal invasive surgery, choledochal cysts have traditionally been treated with open approach. However, with the advancement of technology, minimal invasive surgery has become the new standard approach, particularly in the large volume centers (3,10). The first successful laparoscopic surgery for choledochal cyst was performed in 1995 by Dr. Farello (12), but the adaptation of using laparoscopic approach to perform hepatobiliary surgery has been slow due to the technical complexities of these procedures. The limitation of laparoscopic instruments includes: rigidity of instrument leading to limited degree of freedom, coupled with the fulcrum effect of laparoscopy and 2-dimensional imaging (1). These might contribute to the lack of popularity using this approach. The introduction of robotic surgical system may overcome these hurdles. The major advantages of robotic surgery are the magnified 3D imaging and the enhanced dexterity of instrument control. The camera is mainly control by the console surgeon with very stable vision and the robotic arms can provide intuitive manipulations with tremor filtration, motion scaling, and articulated wrists that allows high degree of freedom of movement (10,13). Better ergonomics for the surgeons are also an important advantage which would allow the surgeon to sit comfortably at the robot console and make delicate dissection, and precise suturing techniques. Although the total operating time for our first robot-assisted resection of choledochal cysts and hepaticojejunostomy is relatively long, we can expect the operation time will be shorter with more experience in robotic surgery.
Conclusions
Robotic-assisted surgery can be safely applied to the resection of type I choledochal cyst and also provide a complex suturing technique for reconstruction with Roux-en-y hepaticojejunostomy. Although the total operating time for robot-assisted resection of choledochal cysts and hepaticojejunostomy is relatively long with this initial experience, the young lady and family are pleased with the cosmetic results.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Akaraviputh T, Trakarnsanga A, Suksamanapun N. Robot-assisted complete excision of choledochal cyst type I, hepaticojejunostomy and extracorporeal Roux-en-y anastomosis: a case report and review literature. World J Surg Oncol 2010;8:87. [Crossref] [PubMed]
- Kim NY, Chang EY, Hong YJ, et al. Retrospective assessment of the validity of robotic surgery in comparison to open surgery for pediatric choledochal cyst. Yonsei Med J 2015;56:737-43. [Crossref] [PubMed]
- Jang JY, Yoon YS, Kang MJ, et al. Laparoscopic excision of a choledochal cyst in 82 consecutive patients. Surg Endosc 2013;27:1648-52. [Crossref] [PubMed]
- Shimura H, Tanaka M, Shimizu S, et al. Laparoscopic treatment of congenital choledochal cyst. Surg Endosc 1998;12:1268-71. [Crossref] [PubMed]
- Tan HL, Shankar KR, Ford WD. Laparoscopic resection of type I choledochal cyst. Surg Endosc 2003;17:1495. [Crossref] [PubMed]
- Metcalfe MS, Wemyss-Holden SA, Maddern GJ. Management dilemmas with choledochal cysts. Arch Surg 2003;138:333-9. [Crossref] [PubMed]
- Rha SY, Stovroff MC, Glick PL, et al. Choledochal cysts: a ten year experience. Am Surg 1996;62:30-4. [PubMed]
- Woo R, Le D, Albanese CT, et al. Robot-assisted laparoscopic resection of a type I choledochal cyst in a child. J Laparoendosc Adv Surg Tech A 2006;16:179-83. [Crossref] [PubMed]
- Kang CM, Chi HS, Kim JY, et al. A case of robot-assisted excision of choledochal cyst, hepaticojejunostomy, and extracorporeal Roux-en-y anastomosis using the da Vinci surgical system. Surg Laparosc Endosc Percutan Tech 2007;17:538-41. [Crossref] [PubMed]
- Alizai NK, Dawrant MJ, Najmaldin AS. Robot-assisted resection of choledochal cysts and hepaticojejunostomy in children. Pediatr Surg Int 2014;30:291-4. [Crossref] [PubMed]
- Wang SE, Chen SC, Shyr BU, et al. The surgical procedure of robotic assisted excision of type I choledochal cyst with Roux-en-y hepaticojejunostomy reconstruction for a 26-year-old young lady. Asvide 2017;4:576. Available online: http://www.asvide.com/articles/1903
- Farello GA, Cerofolini A, Rebonato M, et al. Congenital choledochal cyst: video-guided laparoscopic treatment. Surg Laparosc Endosc 1995;5:354-8. [PubMed]
- Chang EY, Hong YJ, Chang HK, et al. Lessons and tips from the experience of pediatric robotic choledochal cyst resection. J Laparoendosc Adv Surg Tech A 2012;22:609-14. [Crossref] [PubMed]