Robot-assisted minimally invasive procedures for complicated biliary stone disease
Introduction
A big advancement in endoscopic management for biliary stone diseases was seen in the past three decades. Bile duct stones can be removed after sphincterotomy or balloon sphincteroplasty with stone basket, balloon or mechanical lithotripsy during endoscopic retrograde cholangiopancreatography (ERCP). In difficult cases, newer technique like per oral cholangioscopy involves the passage of small caliber disposable scope through the working channel of duodenoscope allows stone crushing with laser under direct vision. Surgical means for retrieval of biliary stones also move from open to laparoscopic approach. Conventional laparoscopic approach is usually sufficient to deal with uncomplicated biliary stone disease by means of laparoscopic cholecystectomy and laparoscopic bile duct exploration. Nevertheless, complicated stone diseases still occur which are beyond endoscopic retrieval and are difficult for laparoscopic retrieval. In these technically demanding cases, robot represents a viable option to facilitate the minimally invasive approach. It can provide a steady working platform and facilitate creation and subsequent closure of choledochotomy. Robot also allows high dexterity of instruments even in a limited working space. There is no big specimen for retrieval, thus the small size wounds for the instrument ports can significantly decrease the chance of wound infection and other wound related complications. Here we report our experience in adopting the robot for the management of three complicated biliary stone diseases.
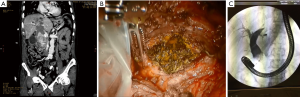
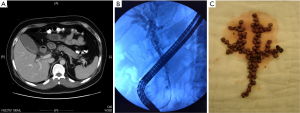
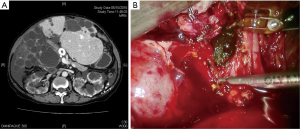
In the first patient, an exceedingly large single common bile duct (CBD) stone 8 cm in largest dimeter was encountered (Figure 1). In the second patient, up to 80 stones of sizes around 3 mm were present in a narrow bile duct (Figure 2). The third patient had underlying polycystic liver disease and gallstone disease complicated with Mirizzi syndrome (Figure 3). Attempts at endoscopic retrieval of biliary stones failed in all three patients. A biliary stent was placed endoscopically. Robot assisted surgery involving cholecystectomy, bile duct exploration, stone retrieval and suturing of bile duct was performed. Additional liver cyst fenestration was done in the third patient.
Surgical technique
The da Vinci S robotic system was used in all three cases. Patient was put in supine position with head up and right side up manner. One 12 mm and three 8 mm robotic ports were inserted in upper abdomen in a semicircular manner with center at right upper quadrant of abdomen. One 12 mm assistant port and one 5 mm assistant port were inserted in lower abdomen, to facilitate suction, traction, passage of needle and small gauze. Operation began with lysis of adhesion around gallbladder (GB) and CBD. In the third case, to facilitate exposure, nearby liver cysts were unroofed with robotic harmonic shear. GB was removed in conventional manner except in the third case it was removed fundus first as a subtotal cholecystectomy was planned for Mirizzi syndrome. Anterior longitudinal choledochotomy was made and CBD stones were removed with robotic forceps and placed in plastic bag in the first two cases (Figure 1B,2C). For the third case, stone could be removed through the GB opening near CBD (Figure 3B). Choledochoscope was inserted through the right side 8 mm robotic port for removal of stones in lower CBD and intrahepatic ducts with the aids of stone basket and balloon. The choledochotomy was closed primarily with 3/0 or 4/0 polydioxanone according to size of CBD. For the third patient, the GB cuff tissue left close to CBD was closed with single layer 3/0 polydioxanone. T-tube was not placed in any of the cases. Drains were placed in all three cases and no postoperative bile leak was noted. ERCP was repeated in the post-operative period to remove the stent and to complete stone clearance in the second and the third patient (Figure 1C). Complete stone clearance was achieved in all three cases and all patients enjoyed the benefits of minimally invasive approach.
Discussion
Robot assisted CBD exploration was scarcely reported in the literature. The first robot assisted choledochotomy was reported in 2004 (1). The closure of choledochotomy involved the insertion of a kehr drain and suturing of bile duct. The second case was reported in 2008. It involved the use of a T-tube for closure of choledochotomy (2). In 2013, the same group published a series of 19 robotic versus 18 open CBD exploration for choledocholithiasis (3). T-tube was used in 11 out of 19 patients in the robotic arm. The robotic group had a longer operating time (220±41.26 vs. 169±65.81 min) but the median hospital stay was shorter (4 vs. 11 days). There was no difference in mortality or morbidity rate. Another series of 5 cases of robotic-assisted cholecystectomy and CBD exploration was reported in 2011 (4). In this last series, the stone size ranged from 5 to 11 mm and number of stones from 1 to 7. The bile duct was closed primarily without biliary stent. There was no bile leak in the series but a drain was left for up to 4 or 5 days after operation in each patient. The average length of stay was 5.8±2.5 days.
We did not put in any T-tube after bile duct exploration as chance of bile leak is much decreased by the intentionally left behind biliary stent. This was confirmed by our experience of robot-assisted surgery for Mirizzi syndrome (5). The stent can be removed by ERCP 6 to 8 weeks after operation. This also provides a valuable chance to check stone clearance, as in the second and third case residual stone was found and successfully removed endoscopically.
In contrast to previous published robotic cases, the three cases in our series were much more complicated. The first case was a huge CBD stone whilst there were numerous small stones in a narrow CBD in the second case. The third case was a Mirizzi syndrome further complicated by polycystic liver diseases. We believe that whilst ordinary choledocholithiasis could be managed endoscopically, or laparoscopically after failed ERCP, robot should be reserved in more complicated cases as presented here for cost effectiveness. It makes complicated biliary stone diseases remained amenable for minimally invasive approach so that patient can benefit from that. In conclusion, we believe robot plays an important role in the management of complicated choledocholithiasis.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Roeyen G, Chapelle T, Ysebaert D. Robot-assisted choledochotomy: feasibility. Surg Endosc 2004;18:165-6. [Crossref] [PubMed]
- Jayaraman S, Davies W, Schlachta CM. Robot-assisted minimally invasive common bile duct exploration: a Canadian first. Can J Surg 2008;51:E93-4. [PubMed]
- Alkhamesi NA, Davies WT, Pinto RF, et al. Robot-assisted common bile duct exploration as an option for complex choledocholithiasis. Surg Endosc. 2013;27:263-6. [Crossref] [PubMed]
- Ji W, Zhao Z, Dong J, et al. One-stage robotic -assisted laparoscopic cholecystectomy and common duct exploration with primary closure in 5 patients. Surg Laparosc Endosc Percutan Tech 2011;21:123-6. [Crossref] [PubMed]
- Lee KF, Chong CN, Ma KW, et al. A minimally invasive strategy for Mirizzi syndrome: the combined endoscopic and robotic approach. Surg Endosc. 2014;28:2690-4. [Crossref] [PubMed]


