
Can a laparoscopic surgery be an alternative to transjugular intrahepatic portosystemic shunts (TIPS) for the treatment of portal hypertensive bleeding?
We read with great confusion the guidance written by Garcia-Tsao et al. (1). In the practice guidance developed by the American Association for the Study of Liver Diseases (AASLD), there is no trail of surgical operation for the treatment of portal hypertensive bleeding in cirrhosis at all. However, it is well known that surgical shunts played an important role in this setting before the emergence of transjugular intrahepatic portosystemic shunts (TIPS), existing studies have shown that surgical shunt still has better long-term patency and survival than TIPS (2), and surgical portoazygous devascularization is still considered as the most direct and effective way of hemostasis in some countries (3).
It is undeniable that TIPS, EVL and BRTO for the treatment of portal hypertensive bleeding in cirrhosis have less invasion and fewer adverse complications than traditional surgery, which may be the reason why they displace surgery. However, with the development of laparoscopic surgery and the improvement of surgical techniques, surgical operations can also be minimally invasive and have fewer complications.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this article and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
We performed a laparoscopic surgery for a patient with gastroesophageal variceal hemorrhage (GEVH), combining shunt with devascularization, in this operation, the main trunk of the portal vein (PV) and the main trunk of the inferior vena cava (IVC) were directly shunted side-to-side. There was an absolute pressure gradient between them, and there was no graft between them, theoretically, it had the best long-term patency. Then, as using grafts, a restrictive ring was used to limit the anastomotic diameter of the shunt to 8 mm, so that the incidence of hepatic encephalopathy (HE) was low and the liver function was well preserved (4). Moreover, we could safely and easily complete surgical portoazygous devascularization by using Ligasure, and the spleen was retained to reduce the risk of postoperative complications (5). While exceeding the effect of TIPS in reducing the PH, and the effect of EVL or BRTO in local hemostasis, the natural portosystemic shunt blood could be returned to the PV to strengthen PV perfusion, protected liver function and reduced the incidence of HE. Most importantly, this is a minimally invasive surgery (MIS) performed completely under laparoscopy, as well as an economical procedure. We call this surgery as Laparoscopic Limited Portacaval Shunt + Portoazygous Devascularization—LLPSPD (Figure 1).
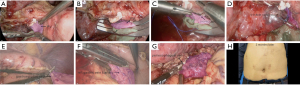
There is an edited video of the surgery available to interested peers (Video 1).
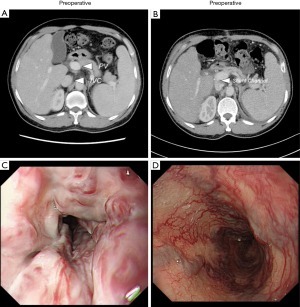
This patient was discharged home 6 days after surgery and had been followed up for 10 months. The enhanced CT and endoscopic examination (6 months after surgery) showed that the shunt channel was patent and the varices were significantly relieved (Figure 2).
In fact, there are still many patients with portal hypertensive bleeding who have no condition for liver transplantation and have difficulties in performing TIPS, can LLPSPD be considered as an alternative treatment?
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was a standard submission to the journal. The article did not undergo external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://hbsn.amegroups.com/article/view/10.21037/hbsn-22-569/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this article and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Garcia-Tsao G, Abraldes JG, Berzigotti A, et al. Portal hypertensive bleeding in cirrhosis: Risk stratification, diagnosis, and management: 2016 practice guidance by the American Association for the study of liver diseases. Hepatology 2017;65:310-35. [Crossref] [PubMed]
- Orloff MJ. Fifty-three years' experience with randomized clinical trials of emergency portacaval shunt for bleeding esophageal varices in Cirrhosis: 1958-2011. JAMA Surg 2014;149:155-69. [Crossref] [PubMed]
- Deng ZC, Jiang WZ, Chen L, et al. Laparoscopic VS. Open splenectomy and oesophagogastric devascularisation for liver cirrhosis and portal hypertension: A retrospective cohort study. Int J Surg 2020;80:79-83. [Crossref] [PubMed]
- Hillebrand DJ, Kojouri K, Cao S, et al. Small-diameter portacaval H-graft shunt: a paradigm shift back to surgical shunting in the management of variceal bleeding in patients with preserved liver function. Liver Transpl 2000;6:459-65. [Crossref] [PubMed]
- Bai DS, Qian JJ, Chen P, et al. Laparoscopic azygoportal disconnection with and without splenectomy for portal hypertension. Int J Surg 2016;34:116-21. [Crossref] [PubMed]


