Emerging new standard for non-invasive assessment of liver disease mortality in non-alcoholic fatty liver disease
We read with great interest the study by Aynur Unalp-Arida and Constance E. Ruhl on hepatic steatosis and mortality in 14,527 adult participants with up to 23 years of linked-mortality data from the U.S. National Health and Nutrition Examination Survey. In the study, severe hepatic steatosis on ultrasonography was found to be associated with increased liver disease mortality (1). It is interesting to note that a study on the same cohort of patients several years earlier found that hepatic steatosis on ultrasonography was not associated with increased liver disease mortality (2). The conflicting result may be partly due to the lower number of liver disease mortality in the earlier study, but more importantly, participants were further categorized according to the severity of hepatic steatosis on ultrasonography in the subsequent study. We know that ultrasonography is not able to distinguish between fatty liver disease patients with and without advanced fibrosis unless there are gross features of cirrhosis. Furthermore, advanced fibrosis will more likely appear as “severe hepatic steatosis” on ultrasonography. Thus, it is possible that the inclusion of participants with advanced fibrosis contributed to the higher liver disease mortality seen in participants with “severe hepatic steatosis” in the subsequent study. It is possible to determine if this was the case by using scores for estimation of fibrosis such as the aspartate aminotransferase (AST) to platelet ratio index, fibrosis-4 or the non-alcoholic fatty liver disease (NAFLD) fibrosis score, which utilizes parameters that appear to be readily available from the dataset.
We know that advanced fibrosis is a strong predictor of liver disease mortality in patients with NAFLD, as has been shown in a meta-analysis of studies with baseline liver biopsy (3), and more recently, in a study on 229 biopsy-proven NAFLD patients after up to 33 years of follow-up (4). Because of the inherent limitations of a liver biopsy procedure and the histopathological examination of the liver biopsy specimen, non-invasive assessment of fibrosis in patients with chronic liver disease, including NAFLD, has gained popularity. In a meta-analysis on 7,058 patients with chronic liver disease of various aetiologies, a higher liver stiffness measurement by elastography was found to be significantly associated with hepatic decompensation, hepatocellular carcinoma, death and a composite of these outcomes (5). A recent study compared liver stiffness measurement by Fibroscan and several blood fibrosis tests for the prognostication of NAFLD patients. In the study, liver stiffness measurement had the highest diagnostic accuracy for advanced fibrosis, and was able to stratify patients into subgroups with significantly different prognoses. The patients were subsequently categorised into four subgroups defined by three thresholds of baseline liver stiffness measurement i.e., 8.8, 12.0 and 38.6 kPa, and the overall survival and survival free of death from liver-related complications were significantly poorer as the liver stiffness measurements increased from one group to another (6). Based on these findings, we believe the use of non-invasive tests such as liver stiffness measurement, will play an important role in the evaluation, prognostication and management of NAFLD patients in the near future. However, as the NAFLD patients who underwent liver biopsy in the study were those who were referred to a specialized hepatology unit, the results could have been affected by selection bias. Thus, it would be best that the findings were further validated in unselected NAFLD patients, bearing in mind that a much larger cohort would be necessary for such a task given the relatively low outcome events in these patients.
Aynur Unalp-Arida and Constance E. Ruhl also noted that elevated serum alanine aminotransferase (ALT) and AST levels were significantly associated with a higher liver disease mortality (1). It is noteworthy that the threshold for elevated serum ALT level and serum AST level was 34 and 30 IU/L, respectively, for men, and 22 and 26 IU/L, respectively, for women, and that these thresholds represented the gender-specific 10th decile of each of the markers in the study. Interestingly, in an earlier study on the same cohort of patients that used a slightly higher laboratory-based threshold for elevated serum ALT and AST levels, 40 and 37 IU/L, respectively, for men, and 31 IU/L for both markers for women, elevated serum ALT and AST levels did not appear to have an impact on mortality (7). This highlights the limitation of these markers for assessment of NAFLD patients, particularly for the diagnosis of non-alcoholic steatohepatitis (NASH). NASH is the more severe form of NAFLD that can lead to fibrosis and cirrhosis, and has been associated with increased liver disease mortality (3). NAFLD comprises of several histological components (8), and these markers may be variably expressed with different severity of each of these histological components, not to mention with different individuals, so much so that having a marker that could accurately characterize an individual patient using a pre-determined threshold is not always possible (9). For example, in a study on 173 biopsy-proven NAFLD patients, serum ALT level was not associated with histological severity, and normal serum ALT level was observed even in patients with NASH and significant fibrosis (10). In a study at our centre, serum AST level was found to have only fair accuracy in discriminating NASH from non-NASH among biopsy-proven NAFLD patients (9). Further analysis revealed that elevated serum AST level, especially when over twice the upper limit of normal, had excellent predictive value for the presence of NASH. However, normal serum AST level had very poor predictive value for the absence of NASH (Table 1).
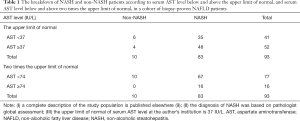
Full table
In conclusion, while an accurate non-invasive test for NASH remains elusive, fairly accurate non-invasive tests such as liver stiffness measurement, are already available for the diagnosis of advanced fibrosis, an important prognostic factor in NAFLD patients. As the data on prognostication of NAFLD patients using these non-invasive tests begin to emerge, less accurate surrogate markers for severe liver disease such as “severe hepatic steatosis” on ultrasonography and elevated serum ALT and AST levels (or rather the lack of elevated serum ALT and AST levels for the diagnosis of less severe liver disease) will likely fall out of favour both in research and in clinical practise.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Unalp-Arida A, Ruhl CE. Noninvasive fatty liver markers predict liver disease mortality in the U.S. population. Hepatology 2016;63:1170-83. [Crossref] [PubMed]
- Kim D, Kim WR, Kim HJ, et al. Association between noninvasive fibrosis markers and mortality among adults with nonalcoholic fatty liver disease in the United States. Hepatology 2013;57:1357-65. [Crossref] [PubMed]
- Musso G, Gambino R, Cassader M, et al. Meta-analysis: natural history of non-alcoholic fatty liver disease (NAFLD) and diagnostic accuracy of non-invasive tests for liver disease severity. Ann Med 2011;43:617-49. [Crossref] [PubMed]
- Ekstedt M, Hagström H, Nasr P, et al. Fibrosis stage is the strongest predictor for disease-specific mortality in NAFLD after up to 33 years of follow-up. Hepatology 2015;61:1547-54. [Crossref] [PubMed]
- Singh S, Fujii LL, Murad MH, et al. Liver stiffness is associated with risk of decompensation, liver cancer, and death in patients with chronic liver diseases: a systematic review and meta-analysis. Clin Gastroenterol Hepatol 2013;11:1573-84.e1-2; quiz e88-9.
- Boursier J, Vergniol J, Guillet A, et al. Diagnostic accuracy and prognostic significance of blood fibrosis tests and liver stiffness measurement by FibroScan in non-alcoholic fatty liver disease. J Hepatol 2016;65:570-8. [Crossref] [PubMed]
- Lazo M, Hernaez R, Bonekamp S, et al. Non-alcoholic fatty liver disease and mortality among US adults: prospective cohort study. BMJ 2011;343:d6891. [Crossref] [PubMed]
- Kleiner DE, Brunt EM, Van Natta M, et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology 2005;41:1313-21. [Crossref] [PubMed]
- Chan WK, Sthaneshwar P, Nik Mustapha NR, et al. Limited utility of plasma M30 in discriminating non-alcoholic steatohepatitis from steatosis—a comparison with routine biochemical markers. PLoS One 2014;9:e105903. [Crossref] [PubMed]
- Wong VW, Wong GL, Tsang SW, et al. Metabolic and histological features of non-alcoholic fatty liver disease patients with different serum alanine aminotransferase levels. Aliment Pharmacol Ther 2009;29:387-96. [Crossref] [PubMed]


