Persistent bronchobiliary fistula managed by endoscopic biliary stenting
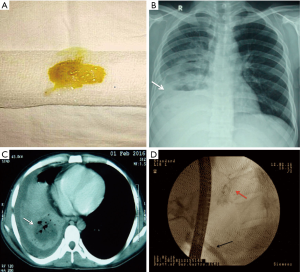
A 26-year-old man presented with right hypochondrium pain, fever and copious greenish-yellow expectoration for 15 days (Panel A). He had undergone laparotomy with peritoneal lavage for ruptured amoebic liver abscess 1 month back.
Chest X-ray showed a homogenous opacity over the right lower zone with pleural effusion (Panel B). CT scan described a trans-diaphragmatic bronchobiliary fistula (BBF) and a large abscess in the right lobe of liver containing fluid and air specks (Panel C).
The patient was initially managed with a right intercoastal drainage tube (ICDT) and percutaneous drainage of liver abscess to which he responded favorably and his sepsis resolved. However, ICDT output remained high (~300 mL/day) even after 2 weeks, indicating chronic BBF. He was taken up for endoscopic biliary decompression. Cholangiogram demonstrated a fistulous connection between bile duct and right bronchial tree (Panel D). Following biliary stenting, both expectoration and chest drain output drastically decreased and resolved completely by day 4.
Acknowledgements
None
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.