Robotic surgery: the promise and finally the progress
It was 1983, when the first experimental surgical robotic operations were performed by McEwen, Auchinlec, and Day on the Arthrobot at the University of British Columbia. The decades that have passed since have seen the SRI International telesurgical system, the PROBOT [1991], the ROBODOC [1992], and other academic and experimental medical robots. Finally, in 1992, Computer Motion Inc. brought the robotic Automated endoscopic system for optimal positioning (AESOP) system to use in the operating room, followed by Intuitive Surgical and its da Vinci surgical system in 2000. The last decade and a half have seen much evolution in the field. The surgical robot evolved from a single purpose robot, to a true surgical instrument with many potential operations. Over one million operations of many types have been performed with the assistance of the surgical robot. Though the field is still in its infancy, the potential impact of this field is starting to be appreciated.
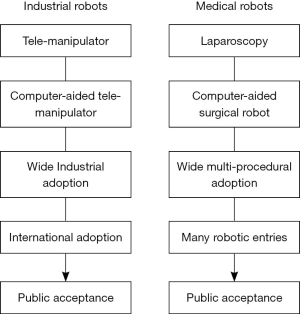
Industrial robots had their birth as mechanical teleoperators for handling radioactive material in the 1940’s. Computer controllers were applied to the teleoperators in the 1950’s. The first Unimation® robots were put to work stacking boxes at General Motors plants in the 1960’s, with Kawasaki licensing the technology in 1968 to start the Japanese entry into robotic development. Fast forward to 2016: robots are now used not only to stack boxes but for many of the essential steps in welding and assembling the over 70 million vehicles produced worldwide yearly (Figure 1). More importantly, there is now general acceptance of robotics for manufacturing. There is also a public acceptance that robots will interact with us in other facets of daily life including in the form of driverless cars.
Surgical robots have a parallel development. Laparoscopes are the mechanical teleoperators in the surgical suite. Placing computerized controls on laparoscopic teleoperators created the current generation of surgical robots. Increasing number of tools and number of robotic entries into the market now allow an increasingly diverse number of procedures to be safely and effectively performed on the robotic platform. We are now at a pivotal point in the field when a technology is about to transform from a tool for innovators and experts to a tool for general practitioners. For hepatobiliary surgery in particular, the progress that has been made in the last five years in robotically-assisted MIS surgery has been astounding. In this issue of HBSN, we have highlighted some of these achievements and future challenges.
One of the most important issues to address now and ongoing is the economics of robotically-assisted surgery. Patti and Ore (1) summarizes the economic status of the field at present. There is no doubt that for most of the operations currently performed by the robotic MIS approach, it takes longer and costs more. The reason that most cars in the world are created by robotically-assisted manufacturing is that it is faster and costs less. Getting to that point in robotic surgery for many operations should be our common goal in this field. Only then will robotically-assisted MIS surgery have long term viability. If new procedures are safer, cheaper, and faster, there would be no calls for randomized control data. Much more expensive interventional radiology (IR) suites are acceptable expenses because the rapid turn-over IR practice and rapid recovery has transformed many morbid procedures with long-hospital stays and rough recovery to a less expensive, rapid recovery, outpatient workflow. There are few randomized trials supporting adoption of most accepted IR procedures.
Patient selection will have an important role to play in shortening operations, decreasing cost, and improving recovery. Operations with minor physiologically deleterious effects that require large incisions for open surgeries are the best cases for robotic MIS surgery. These incision-dominant operations are also those cases that are best for proving better outcome by data. Melstrom et al. (2) present their argument for this point by reporting a series of liver resections where 30% of the patients were outpatients or short-stay patients.
Defining pathways and order sets is another essential part of the data-driven standardization helpful for rapid recovery. Warner et al. (3) present a set of proposed enhanced recovery from surgery (ERAS) pathways based on data and experience. In this paper, they summarize data supporting essential use of fluids, blood, prophylactic medications. Pathways will also help in cost management. If consistent deviation from practice is seen, it will also drive the next generation questions for study.
A most import factor in safe, efficient, and effective robotic-MIS practice is a formalized program with technical support and on-going training. This will be of even greater importance as new robotic platforms enter the market, with new set-ups, work-flows, and instruments will challenge surgeons, teams, and daily routine. The evolution of robotic training and surgery in Hong Kong (4) and South Korea (5) are summarized by Lai and Choi respectively, two pioneers who have built not only flourishing clinical programs but great training facilities. Nota and his colleagues (6) present a Western look at the same issues by summarizing their experience of starting a robotics program at the University of Utrecht.
Some robotic operations are characterized by a long learning curve and long operative time. Some of these operations are described in this issues, including current status of robotic living liver donor harvest (7) and robotic choledochal cyst excision (8). Operative approaches that cost more and takes longer will have to have substantial proven benefit to be accepted. These operations should be concentrated at high volume centers, where surgical expertise as well as patient volume optimizes outcomes.
The prospects for robotic MIS surgery are bright. For common low-intensity operations, we need to make it safer, faster, cheaper, or easier (9). For high-end technical operations, we need to work on technical enhancements and workflows that substantially improve outcome or enable new operations. Most importantly we need to enhance training. We need to train our expert robotic surgeons to be innovators, retaskers, and paradigm changers. We need to train high-volume surgeons to be efficient, safe, cost-conscious robotic surgeons. We need to train our resident and fellows to be expert surgeons with surgical robots as a routinely used tool in their armamentarium. We need to evolve tools, workflow, workforce, and paradigm to optimize value and outcome for our surgical patients.
Acknowledgements
None.
References
- Patti JC, Ore AS, Barrows C, et al. Value-based assessment of robotic pancreas and liver surgery. HepatoBiliary Surg Nutr 2017;6:246-57.
- Melstrom LG, Warner SG, Woo Y, et al. Selecting incision-dominant cases for robotic liver resection: towards outpatient hepatectomy with rapid recovery.
- Warner SG, Jutric Z, Nisimova L, et al. Early recovery pathway for hepatectomy: data-driven liver resection care and recovery. HepatoBiliary Surg Nutr 2017. [Epub ahead of print].
- Lai EC, Tang CN. Training robotic hepatectomy: the Hong Kong experience and perspective. HepatoBiliary Surg Nutr 2017;6:222-9.
- Choi GH, Chong JU, Han DH, et al. Robotic hepatectomy: the Korean experience and perspective. HepatoBiliary Surg Nutr 2017;6:230-8.
- Nota CL, Borel Rinkes IH, Hagendoorn J. Setting up a robotic hepatectomy program: a Western- European experience and perspective. HepatoBiliary Surg Nutr 2017;6:239-45.
- Chen P, Wu C, Wu Y. Use of robotics in liver donor right hepatectomy. HepatoBiliary Surg Nutr 2017. [Epub ahead of print].
- Wang S, Chen S, Shyr B, et al. Robotic assisted excision of type I choledochal cyst with Roux-en-y hepaticojejunostomy reconstruction. HepatoBiliary Surg Nutr 2017. [Epub ahead of print].
- Zaman JA, Singh PT. The emerging role for robotics in cholecystectomy: the dawn of a new era? HepatoBiliary Surg Nutr 2017. [Epub ahead of print].