
Health-related quality of life of living liver donors 1 year after donation
Introduction
Living-donor liver transplantation (LDLT) is one means of addressing organ shortages in liver transplantation and has become a life-saving therapy for patients with end-stage liver disease worldwide (1,2). However, living liver donors often experience considerable physiological, psychological, and social changes following surgery, which require the attention of the transplant team (3,4). An important goal of such post-donation care is to help donors regain their health and quality of life. Health-related quality of life (HRQOL) can be defined as well-being in the physical, psychological, social, and environmental domains of life, and it is an important indicator of the quality of medical care. Cross-sectional studies have indicated that although most donors maintain an above-average HRQOL after the donation, some report markedly poorer HRQOL or perceive their health to be worse than before the donation (5-8). Prospective studies have reported that the physical domain of HRQOL is the most affected in the earliest stages after donation, although it may return to pre-donation levels within 6 to 12 months after donation (8-10). Still, the HRQOL of living liver donors requires more investigation, and a prospective study design is perhaps best suited to understanding the changes in HRQOL after donation.
Investigating the predictors of HRQOL is also important for identifying high-risk groups and promoting donors’ overall welfare. Although a number of risk factors have been identified, such as post-donation complications, recipient mortality, and the donors’ social and demographic characteristics, studies on them have yielded inconsistent conclusions (3,7,8). Some living liver donors reportedly experience ambivalence (i.e., the coexistence of inconsistent or opposing perceptions) before donation (11), which may affect their physical and mental health thereafter. However, the relationship between pre-donation ambivalence and post-donation HRQOL had not been thoroughly investigated. Another factor that potentially influences the HRQOL of living organ donors is the sense of coherence (12). Sense of coherence is defined as “a resource that enables people to manage tension, to reflect about their external and internal resources, to identify and mobilize them, to promote effective coping by finding solutions, and resolve tension in a health promoting manner ” (13). Individuals with a strong sense of coherence may feel that their life is meaningful and that their stress is understandable and manageable (13). However, no studies have yet examined the effect of sense of coherence on HRQOL of living liver donors, suggesting that the association between sense of coherence and HRQOL needs further investigation.
Investigating the HRQOL and influencing factors of living liver donors pre- and post-donation may help enrich our understanding of their quality of life as well as promote the quality of their care. Given the prevalence of LDLT in Asian countries (14), it is a research avenue worth pursuing. The purpose of this study was to assess the HRQOL of living liver donors and analyze the effects of pre-donation ambivalence, sense of coherence, post-donation complications, and recipient mortality, as well as donors’ and recipients’ basic characteristics, on the HRQOL of living liver donors up to 1 year after donation.
Methods
Study design and participants
We used a prospective, correlational design in this study. The data were collected at pre-donation and at 1, 3, 6, and 12 months post-donation from living liver donors. The inclusion criteria for this study were age of 20 years or older and having donated part of their liver to an adult recipient.
All pre-donation information was collected during candidacy assessments in the clinic of a medical center in northern Taiwan. We explained the purpose and data collection process to potential participants and obtained their written informed consent. They were also assured of their right to refuse participation or to withdraw from the study at any stage. After the donation, we mailed a set of self-administered questionnaires with a stamped envelope to the participants. They were encouraged to return these questionnaires within 3 days. Up to 2 text reminders were sent to participants if they did not return the questionnaires within the recommended time frame. Numerical codes were used in place of the participants’ names. This study conformed to the ethical guidelines of the 1975 Declaration of Helsinki. The data collection was approved by the Chang Gung Medical Foundation Institutional Review Board (approval No. CGMH 102-1974B).
Measures
The Chinese version of the Medical Outcomes Study 36-Item Short Form Survey (SF-36) was used to assess HRQOL (15). This questionnaire is a widely used instrument that has been validated for assessing the HRQOL of organ transplant recipients (16). The scale contains 36 items in 8 subscales: physical functioning, role-physical, bodily pain, general health, vitality, social functioning, role-emotional, and mental health (17). The internal consistency reliability (Cronbach’s α) of the 8 subscales ranged from 0.54 to 0.91 in this study. These 8 subscales can in turn be merged into 2 dimensions: the physical (PCS) and mental (MCS) component summary (17). To aid in our understanding of overall HRQOL, we employed the PCS and MCS scores for the statistical analysis in this study. For this scale, higher scores indicated better HRQOL.
The ambivalence subscale of the Donor Attitude Scale developed by Simmons et al. was used to measure participants’ level of pre-donation ambivalence (18). This subscale contains 7 items. One item (“Did you know right away you would definitely do it, or did you think it over?”) is answered on a dichotomous scale, where a response of 0 indicates that the decision was made instantly and a response of 1 indicates that the decision required thought. The other 6 items use a 4-point Likert scale, which were subsequently recoded by us into a dichotomous scale. For example, for the item “How hard was the decision to make?”, the response options included “very hard”, “somewhat hard”, “a little hard” or “not at all hard” If the answer was “very”, “somewhat” or “a little”, the participants were given a score of 1; if their answer was “not at all hard,” then the score was 0 because the answer indicated no ambivalence. A possible score was 0–7, with higher scores indicating a higher degree of ambivalence. The Chinese version of the ambivalence subscale was developed by translating the original, and permission for its use was obtained (19). This scale has been used to assess living liver donor candidates (20,21). The internal consistency reliability (Cronbach’s α) was 0.71 in this study.
The 13 items of the Chinese version of the Sense of Coherence Scale were used to measure sense of coherence in this study (22). Sample items for this scale include “Doing the things you do every day is: (from ‘a source of deep pleasure and satisfaction’ to ‘a source of pain and boredom’)” and “Do you have a feeling that you are in an unfamiliar situation and don’t know what to do? (from ‘very often’ to ‘very seldom or never’)”. The responses were made on a 7-point Likert scale; thus, the possible total score range is 13–91. Higher scores indicate a higher level of sense of coherence. The internal consistency reliability (Cronbach’s α) was 0.84 in this study.
We also obtained donors’ basic information, including their age, sex, marital status, education level, and relation to recipients. The recipients’ information, which we also assessed, included age, sex, Model for End-Stage Liver Disease (MELD) score, and survival status at 1 year after surgery. We used the Clavien classification system (grades I–V), drawing on information from donors’ medical records, to assess post-donation complications in donors (23,24). In the multivariate analysis, we classified donors into 2 groups based on whether or not they experienced complications.
Statistical analysis
The data analyses were performed using SPSS Statistics version 20.0 (IBM Corp., Armonk, NY, USA). Descriptive statistics including means, standard deviations (SD), and ranges were calculated for continuous data, whereas frequencies and percentages were calculated for categorical data. The linear mixed model (LMM) was used to examine the change in HRQOL and determined the predictors of HRQOL after donation. The LMM is considered useful for understanding changes in study variables over time and examining the effects of influencing factors (25). First, the effect of the pre-donation variables (e.g., demographic characteristics, donors’ pre-donation ambivalence, donors’ sense of coherence, recipients’ MELD score) on HRQOL were analyzed. Second, the effects of the post-donation variables (e.g., donors’ complication and mortality of recipients) were analyzed. Finally, if any pre- or post-donation variables showed statistical significance (P<0.05), these factors were included in the final multivariate model. The PCS and MCS scores at pre-donation were placed in each model to serve as control variables. The significance level (P value) was set at <0.05.
Results
One hundred thirty-five donors underwent a right-lobe hepatectomy for LDLT during the enrollment period (August 2013 to December 2015). Of them, 102 agreed to participate in this study. Those who refused to participate did so because of a “busy schedule” and “no interest”. Of these 102 enrolled donors, 68 patients (66.7%) completed the questionnaire five times after the donation and were analyzed in this study. There were no statistically significant differences between the donors that completed the follow-up questionnaires and those who did not in terms of age (P=0.87), sex (P=0.89), relation to recipients (P=0.93), sense of coherence (P=0.28), pre-donation ambivalence (P=0.41), post-operation complication (P=0.67), and recipients’ survival status (P=0.11) (data not shown).
The mean age of the 68 donors was 31.6 years, and 54.4% were female. Most of the donors were single, had a bachelor’s degree education, and had donated part of their liver to their parents. Meanwhile, the mean age of the recipients was 55.1 years, and most were male (73.5%). Their mean MELD score was 17.29, and 58 (85.3%) of the recipients survived the first year after surgery. The mean ambivalence score was 3.96 (SD =1.77); this indicated that donors experienced moderate ambivalence pre-donation. Their mean sense of coherence score was 63.16 (SD =12.29), indicating that donors had fairly high psychological strength and resources for coping with stress (Table 1).
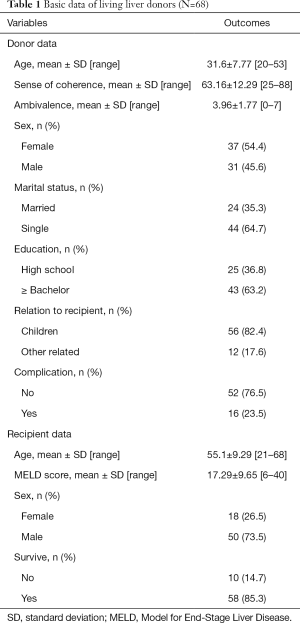
Full table
Sixteen (23.5%) donors were found to have experienced mild complications according to the Clavien classification system, with 9 donors having a grade of I and 7 donors having a grade of II. The remaining donors experienced no complications. No donors died as a result of the operation (Table 2).

Full table
The mean PCS score ranged from 43.59 to 56.70 throughout the study. It tended to be worse (compared to pre-donation) at 1 month after donation (mean =43.59, SD =7.06), but returned to around pre-donation levels at 12 months after donation. The mean MCS score was quite constant across the study period, ranging from 45.80 to 46.89 (Table 3).
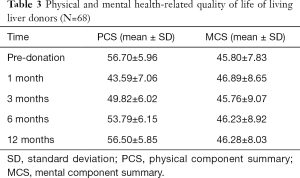
Full table
According to the LMM, the PCS score was significantly worse at 1 month (coefficient =−13.52, P<0.01) after the donation; however, it showed a trend toward improvement as time passed (i.e., the coefficients improved). None of the pre-donation variables had a significant effect on PCS score. However, donors’ complication after the donation had a significant influence on the PCS score: that is, donors who did not experience a complication had better PCS scores than did donors who experienced a complication (coefficient =2.83, P=0.02) (Table 4).
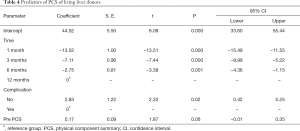
Full table
As for the MCS, the LMM (Table 5) shows that the MCS score remained relatively constant over time (P>0.05). Both pre-donation (donors’ education level and recipients’ MELD score) and post-donation (recipients’ survival status) factors had significant effects on MCS score. Accordingly, these 3 variables were analyzed together in the final LMM. The results showed that all 3 variables remained significant. Specifically, the factors associated with poor MCS scores included an education level of less than a bachelor’s degree (coefficient =−3.60, P=0.004), recipients having a high MELD score (coefficient =−0.13, P=0.03), and recipient death within 1 year after donation (coefficient =−3.48, P=0.03). The pre-donation MCS score was also significantly associated with post-donation MCS score (coefficient =0.39, P<0.001).
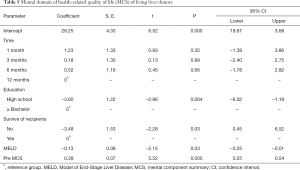
Full table
Discussion
The PCS score was much lower early in the post-donation period, whereas the MCS score remained stable over time. Only post-donation complications were significantly associated with the PCS, whereas 3 factors—education level, recipients’ MELD score, and recipient survival status—were significantly associated with the MCS score.
The pattern in HRQOL in this study was similar to that found in previous reports (7-10). It is understandable that the physical domain of HRQOL of living liver donors would be influenced by the donation, given that donors often experience wound pain, fatigue, diarrhea, and inadequate nutrient intake problem at the early stage after donation (26-28). The mental domain of HRQOL was not significantly influenced by the donation. Donors may believe that the liver donation would helpful for the recipients and other family members, and the psychological benefit may help them maintain a stable mental status. Living-organ transplantation aims to maximize the balance between the safety of living donors and the success of recipients. Living liver donors should undergo careful pre-donation psychosocial assessment (29-31). Donors who have poor mental status would be excluded from the candidacy. The stability of the MCS of living liver donors after surgery is also important. Thus, the care of living liver donors appears to be a continuous process from pre-donation to post-donation.
Post-donation complications were a significant predictor of the PCS score, even though the majority of individuals with post-donation complications in our study participants had mild complications, and none of the donors had life-threatening complications. This finding agrees with a previous report showing that surgical complications can aggravate distress symptom, compromise physical function and daily activity, and influence HRQOL after donation (6,31).
Donors who had a higher education level had higher MCS scores. Ladner et al. found that education less than a bachelor’s degree was a significant predictor of a poor MCS score (8). Patients with higher education can comprehend the extent and consequences of donation more precisely (8) and therefore are better able at coping with surgical trauma. Well-educated donors may also learn the necessary skills for pre-operative preparation, post-operative self-care, and stress coping. Additionally, a higher education level is correlated with higher socioeconomic status and more social resources (32). Good preparation and adequate support resources are considered cornerstones of recovery from major surgery. Health-care professionals in the transplantation team should therefore be attentive to donors’ level of readiness, particularly among those with low education levels. Pre-donation informed consent and post-donation care instructions should be appropriate for the health literacy of donors (8,33).
The recipients’ MELD score (i.e., their disease severity) and recipient death were both negatively correlated with MCS score. When someone experiences severe illness, it can be highly stressful for other family members (31,34,35). In LDLT, recipients and donors are generally from the same family and have close relationships. Accordingly, any sign of deterioration in the recipients’ condition may have a major influence on the donor. Similarly, when a recipient dies after surgery, donors may feel guilty. Therefore, we recommend that health-care professionals pay particular attention to donors whose recipients have a critical illness, as well as provide appropriate grief counseling and follow-up care on mental well-being for donors whose recipients die within 1 year of surgery.
Notably, the level of pre-donation ambivalence had no significant impact on the patients’ HRQOL. One of the important goals of evaluation before donation is to confirm whether the donor is ambivalent about the donation procedure (36). If a donor is extremely ambivalent about the donation, it is advised that they do not undergo the surgery (36). Participants in this study were actual donors; as such, they had undergone careful pre-donation assessment by physicians, psychiatrists, and social workers. This suggests that they had a certain level of psychological, physical, and social readiness. If the donor is sufficiently mentally prepared and has decided to undergo surgery themselves, then it is possible that their quality of life will not be significantly affected by pre-donation ambivalence. Ambivalence is also shown to be a deliberate process, whereby donors tend to balance the pros and cons of living organ donation (37). As such, health-care professionals should help donors through this decision-making process.
Sense of coherence was also not a significant predictor of HRQOL in this study, which does not align with previous reports (12,38). The lack of an association might be because the sense of coherence scores of our participants was already high (i.e., a ceiling effect). Still, it is recommended that health-care personnel encourage donors to use appropriate coping strategies, as well as internal and external resources, to ensure good-quality donor care. The association between individuals’ coping ability and HRQOL warrants investigation in the future.
This study had a high participant attrition, but the sample characteristics did not significantly differ between the participants who completed the study and those who dropped out. Only patients with complete data sets were analyzed in this study. To prevent attrition in future longitudinal studies with repeated measures, electronic versions of the questionnaire with a reminder function should be used. The generalizability of this study’s results should be interpreted with caution since the study was conducted in only a single center with a small number of participants. Future study should include multiple centers and with larger-scale sample.
In summary, the impact of living liver donation on the HRQOL of donors was greatest early on in the post-donation period for the physical domain. Health-care professionals should carefully manage and monitor the prevalence and severity of surgical complication as well as make efforts to identify high-risk groups, including donors with low education levels and donors whose recipients have a severe illness or have died in the first year after surgery.
Acknowledgements
Funding: This work was supported by the Ministry of Science and Technology of Taiwan (Fund Number: MOST 106-2314-B-182-007-MY, NMRPD1G1271).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the Chang Gung Medical Foundation Institutional Review Board (No. CGMH 102-1974B).
References
- Pillai VG, Chen CL. Living donor liver transplantation in Taiwan—challenges beyond surgery. Hepatobiliary Surg Nutr 2016;5:145-50. [PubMed]
- Nydam TL, Reddy MS, Pomfret EA, et al. Progression of living liver donation worldwide. Curr Opin Organ Transplant 2018;23:162-8. [PubMed]
- Dew MA, Butt Z, Humar A, et al. Long-term medical and psychosocial outcomes in living liver donors. Am J Transplant 2017;17:880-92. [Crossref] [PubMed]
- DiMartini A, Dew MA, Liu Q, et al. Social and financial outcomes of living liver donation: a prospective investigation within the adult-to-adult living donor liver transplantation cohort study 2 (A2ALL-2). Am J Transplant 2017;17:1081-96. [Crossref] [PubMed]
- Parikh ND, Ladner DP, Abecassis M, et al. Quality of life in donors after living donor liver transplantation: A review of the literature. Liver Transpl 2010;16:1352-8. [Crossref] [PubMed]
- Takada Y, Suzukamo Y, Oike F, et al. Long-term quality of life of donors after living donor liver transplantation. Liver Transpl 2012;18:1343-52. [Crossref] [PubMed]
- Dew MA, DiMartini AF, Ladner DP, et al. Psychosocial outcomes 3 to 10 years after donation in the adult to adult living donor liver transplantation cohort study. Transplantation 2016;100:1257-69. [Crossref] [PubMed]
- Ladner DP, Dew MA, Forney S, et al. Long-term quality of life after liver donation in the adult to adult living donor liver transplantation cohort study (A2ALL). J Hepatol 2015;62:346-53. [Crossref] [PubMed]
- Ishizaki M, Kaibori M, Matsui K, et al. Change in donor quality of life after living donor liver transplantation surgery: a single-institution experience. Transplant Proc 2012;44:344-6. [Crossref] [PubMed]
- Kroencke S, Nashan B, Fischer L, et al. Donor quality of life up to two years after living donor liver transplantation: a prospective study. Transplantation 2014;97:582-9. [Crossref] [PubMed]
- Steele CI, Altholz JA. Donor ambivalence: a key issue in families of children with end-stage renal disease. Soc Work Health Care 1987;13:47-57. [Crossref] [PubMed]
- Erim Y, Beckmann M, Kroencke S, et al. Sense of coherence and social support predict living liver donors’ emotional stress prior to living-donor liver transplantation. Clin Transplant 2008;22:273-80. [Crossref] [PubMed]
- Eriksson M, Lindström B. Antonovsky’s sense of coherence scale and the relation with health: a systematic review. J Epidemiol Community Health 2006;60:376-81. [Crossref] [PubMed]
- Chen CL, Kabiling CS, Concejero AM. Why does living donor liver transplantation flourish in Asia? Nat Rev Gastroenterol Hepatol 2013;10:746-51. [Crossref] [PubMed]
- Lu JF, Tseng HM, Tsai YJ. Assessment of health-related quality of life in Taiwan (I): development and psychometric testing of SF-36 Taiwan version. Taiwan J Publ Health 2003;22:501-11.
- Jay CL, Butt Z, Ladner DP, et al. A review of quality of life instruments used in liver transplantation. J Hepatol 2009;51:949-59. [Crossref] [PubMed]
- Ware JE Jr, Kosinski M. SF-36 Physical and Mental Health Summary Scales: A Manual for Users of Version 1. 2nd ed. Lincoln, RI: QualityMetric, Inc., 2005.
- Simmons R, Marine S, Simmons RL. Gift of Life: The Effect of Organ Transplantation on Individual, Family, and Societal Dynamics. New Brunswick, NJ: Transaction Books, 1987.
- Liao SC, Lee MB, Lee YJ, et al. Association between quality of informed consent and pre-operation ambivalence. J Med Edu 2005;9:80-90.
- DiMartini A, Cruz RJ Jr, Dew MA, et al. Motives and decision making of potential living liver donors: comparisons between gender, relationships and ambivalence. Am J Transplant 2012;12:136-51. [Crossref] [PubMed]
- Lai YC, Lee WC, Juang YY, et al. Effect of social support and donation-related concerns on ambivalence of living liver donor candidates. Liver Transpl 2014;20:1365-71. [Crossref] [PubMed]
- Tang ST, Dixon J. Instrument translation and evaluation of equivalence and psychometric properties: the Chinese sense of coherence scale. J Nurs Meas 2002;10:59-76. [Crossref] [PubMed]
- Clavien PA, Camargo CA Jr, Croxford R, et al. Definition and classification of negative outcomes in solid organ transplantation. Application in liver transplantation. Ann Surg 1994;220:109-20. [Crossref] [PubMed]
- Liu B, Yan LN, Li J, et al. Using the Clavien grading system to classify the complications of right hepatectomy in living donors. Transplant Proc 2009;41:1703-6. [Crossref] [PubMed]
- Shek DT, Ma C. Longitudinal data analyses using linear mixed models in SPSS: concepts, procedures and illustrations. ScientificWorldJournal 2011;11:42-76. [Crossref] [PubMed]
- Holtzman S, Clarke HA, McCluskey SA, et al. Acute and chronic postsurgical pain after living liver donation: incidence and predictors. Liver Transpl 2014;20:1336-46. [Crossref] [PubMed]
- Humphreville VR, Radosevich DM, Humar A, et al. Long-term health-related quality of life after living liver donation. Liver Transpl 2016;22:53-62. [Crossref] [PubMed]
- Wang SH, Ming YZ, Lin PY, et al. Predictors of diarrhea after hepatectomy and its impact on gastrointestinal quality of life in living donors. PloS One 2016;11:e0166576. [Crossref] [PubMed]
- Schulz KH, Kroencke S, Beckmann M, et al. Mental and physical quality of life in actual living liver donors versus potential living liver donors: a prospective, controlled, multicenter study. Liver Transpl 2009;15:1676-87. [Crossref] [PubMed]
- Dew MA, Zuckoff A, DiMartini AF, et al. Prevention of poor psychosocial outcomes in living organ donors: from description to theory-driven intervention development and initial feasibility testing. Prog Transplant 2012;22:280-92. [Crossref] [PubMed]
- Kousoulas L, Emmanouilidis N, Klempnauer J, et al. Living-donor liver transplantation: impact on donor's health-related quality of life. Transplant Proc 2011;43:3584-7. [Crossref] [PubMed]
- Ross CE, Van Willigen M. Education and the subjective quality of life. J Health Soc Behav 1997;38:275-97. [Crossref] [PubMed]
- Gordon EJ, Daud A, Caicedo JC, et al. Informed consent and decision-making about adult-to-adult living donor liver transplantation: a systematic review of empirical research. Transplantation 2011;92:1285-96. [Crossref] [PubMed]
- Fujita M, Akabayashi A, Slingsby BT, et al. A model of donors' decision-making in adult-to-adult living donor liver transplantation in Japan: having no choice. Liver Transpl 2006;12:768-74. [Crossref] [PubMed]
- Muto K. Organ transplantation as a family issue: living liver donors in Japan. Int J Jpn Sociol 2010;19:35-48. [Crossref]
- Erim Y, Beckmann M, Valentin-Gamazo C, et al. Selection of donors for adult living-donor liver donation: results of the assessment of the first 205 donor candidates. Psychosomatics 2008;49:143-51. [Crossref] [PubMed]
- Simpson MA, Kendrick J, Verbesey JE, et al. Ambivalence in living liver donors. Liver Transpl 2011;17:1226-33. [Crossref] [PubMed]
- Papachristou C, Walter M, Frommer J, et al. A model of risk and protective factors influencing the postoperative course of living liver donors. Transplant Proc 2009;41:1682-6. [Crossref] [PubMed]


