
Alcohol consumption as a cause of cancer: urging for more mechanism study
Alcohol consumption is a major health problem worldwide. It has been identified as a Group 1 carcinogen to humans by The International Agency for Research on Cancer (IARC) in 2006, yet up to 38.1% of the world’s population aged above 15 years old are regular drinkers. Globally, estimates suggest that 5.5% of cancer cases and 5.8% of cancer-related deaths are attributable to alcohol drinking (1). Epidemiologic studies unequivocally acknowledge chronic alcohol drinking as an important risk factor for different types of cancers, including those of upper aerodigestive tract (UADT) (oral cavity, pharynx, larynx and esophagus), liver, pancreas, female breast, colon and blood. However, there are studies suggest that light-to-moderate alcohol drinking appears to trigger anti-inflammatory mechanisms, reducing the risk of coronary heart disease and dementia, and provides protection against type II diabetes (2). And in traditional Chinese medicine (TCM), wine, a popular alcohol beverage, is considered rather beneficial in health preservation.
A number of studies of alcohol drinking have demonstrated that the risk of developing UADT cancers increases significantly even at moderate daily doses. With higher dose of alcohol intake, the risk of UADT cancers increases four to six times. Compared with nondrinkers, people who regularly drink alcohol 50 g per day promotes the risk of esophageal cancer by two to three-fold (3). Alcohol intake is associated with an elevated risk of a second primary cancers in patients with UADT cancers. Besides, alcohol intake has been regarded as one of the leading causes of chronic liver diseases and hepatocellular cancer (HCC) via either direct (genotoxic) or indirect mechanisms (cirrhosis) (4,5). Liver injuries caused by alcohol range from fatty liver, alcoholic steatohepatitis to cirrhosis. It’s the most common cause of HCC (account for 32% to 45% of HCC) in western counties in a dose-dependent fashion. In addition, studies have illustrated that a dose-risk relationship between chronic alcohol consumption and breast cancer in pre- and post-menopausal women. Possibly, increased level of estrogen, which leads to enhanced mammary gland susceptibility to carcinogenesis, is responsible for breast cancer in women consuming alcohol. A recent study found that the risk of all subtypes of breast cancer [luminal A, luminal B, hormone-receptor-negative, HER2-negative (TNBC)] significantly elevated with increasing alcohol intake (6). Furthermore, alcohol intake is also considered a risk for pancreatic cancer. A number of prospective cohort and controlled studies have verified underlying relationship between alcohol drinking and pancreatic cancer. Researchers have found that heavy alcohol drinking is highly correlated with the development of pancreatic cancer, yet low-to-moderate alcohol intake was not significantly associated with the risk of pancreatic cancer. Nonetheless, chronic alcohol drinking is a known risk factor for pancreatitis, and the latter predispose pancreatic cancer. Also, there are verified risks for colorectal cancer concerning alcohol consumption. A pooled analysis found an increased colorectal cancer risk (45% for colon and 49% for rectal cancers) for those who drink alcohol more than 45 g per day, compared with nondrinkers (7). Moreover, alcohol is also a suspected carcinogen for lung cancer, cutaneous melanoma and various hematological cancers, such as lymphoma and leukemia. Although current evidence is not conclusive, it arouses deep consideration of alcohol as a risk factor in the etiology of those cancers.
Alcohol was not considered a carcinogen previously, since it cannot induce cancer when given alone. However, about a decade ago, multiple experiments fed mice and rats with alcohol in their drinking water and recognized ethanol as a direct carcinogen. Yet the mechanism by which alcohol induces cancer is not fully understood. Possible pathways are as follows: genotoxic effect of acetaldehyde, increased estrogen concentration, cellular stress, changes in folate metabolism and inflammation. Several genetic variants have been indicated as candidates for susceptibility in alcohol-induced cancers, such as ADH1B, ADH1C, ALDH2, CYP2E1 and MTHFR. Excessive ethanol results in global DNA hypomethylation and promoter region hypermethylation. Aberrant methylation affects the expression of genes involved in cell cycle, DNA damage repair and tumour suppression. Besides, by interfering estrogen metabolism and generating large amount of reactive oxygen species, alcohol promotes carcinogenesis, migration and invasion of certain cancer. The compromised retinoid signaling and the consequently influenced signaling pathway may also contribute to carcinogenesis. Furthermore, recent studies implicate the microbiome as novel potential mechanisms. Alcohol intake also interferes with various aspects of innate and adaptive immune systems and diminishes immune surveillance to promote cancer development (Table 1).
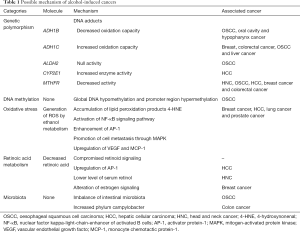
Full table
In conclusion, numerous evidences have demonstrated an association between alcohol drinking and cancers of different organs. Although it seems the harm of alcohol depends on dose, studies that suggest light alcohol drinking is harmless or even beneficial in certain diseases are rather ambiguous. In TCM, wine is considered the essence of grains, and it’s one kind of peculiar “food” with both material and spiritual attributes. It’s regarded as a compound with unique function like regulating qi and health preservation, and it’s conducive to longevity. Further studies are required to explore the possible effects of alcohol beverages on human body, especially the biological mechanisms of alcohol-induced cancers. Since the increasing population of adolescent drinking and binge drinking among youngsters, the public should take this issue more seriously, just like the recommendation in the revised European Code against Cancer (ECAC) fourth edition by IARC in 2016: “If you drink alcohol of any type, limit your drinking. Not drinking is better for cancer prevention”.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Praud D, Rota M, Rehm J, et al. Cancer incidence and mortality attributable to alcohol consumption. Int J Cancer 2016;138:1380-7. [Crossref] [PubMed]
- Metcalf PA, Scragg RK, Jackson R. Light to moderate alcohol consumption is protective for type 2 diabetes mellitus in normal weight and overweight individuals but not the obese. J Obes 2014;2014:634587. [Crossref] [PubMed]
- Li Y, Mao Y, Zhang Y, et al. Alcohol drinking and upper aerodigestive tract cancer mortality: a systematic review and meta-analysis. Oral Oncol 2014;50:269-75. [Crossref] [PubMed]
- Pirola CJ, Sookoian S. The natural history of nonalcoholic fatty liver disease: mortality rates and liver enzymes. Hepatobiliary surgery and nutrition 2017;6:130-4. [Crossref] [PubMed]
- Testino G. The burden of cancer attributable to alcohol consumption. Maedica 2011;6:313-20. [PubMed]
- Gago-Dominguez M, Castelao JE, Gude F, et al. Alcohol and breast cancer tumor subtypes in a Spanish Cohort. SpringerPlus 2016;5:39. [Crossref] [PubMed]
- Fedirko V, Tramacere I, Bagnardi V, et al. Alcohol drinking and colorectal cancer risk: an overall and dose-response meta-analysis of published studies. Ann Oncol 2011;22:1958-72. [Crossref] [PubMed]


