
Influence of the body mass index on postoperative outcome and long-term survival after pancreatic resections in patients with underlying malignancy
Introduction
Pancreatic ductal adenocarcinoma (PDAC) is the 4th leading cause of cancer deaths and is projected to become the second by 2030 (1). Despite advances in the treatment and management of this malignancy, the overall five-year survival rate remains only 5–7% and one-year survival is achieved in less than 20% of patients (2). As patients who have early-stage disease are often those with the best outcomes (3) increased attention has been paid to known risk factors for this disease including family history, diabetes and obesity (4). Obesity is a known risk factor for the development of PDAC (5-7) while underweight has a negative impact on morbidity in patients with a known diagnosis of PDAC (8,9). Overweight and obesity are currently linked to more deaths worldwide than underweight and the prevalence of obesity is rising (10,11). The most commonly used indicator of weight in healthcare is the body mass index (BMI); the WHO defines obesity as a BMI ≥30 while a BMI <18.5 is defined as underweight. Many studies have observed the relationship between body mass and surgical morbidity and mortality; however, the data available remain controversial. Interestingly, in specific conditions a decrease in mortality has been reported in overweight patients: this is the case of patients with septic shock (12) and acute respiratory distress syndrome (13) and is referred to as the obesity paradox. While the long-term survival rate among patients with periampullary carcinomas remains low (14), it can be influenced by various factors. Some recent reports show that being overweight or obese correlates with a lower risk for hospital mortality and a lower risk of adverse postoperative outcomes (15). The purpose of this retrospective study was to quantify the effects of body mass on postoperative complications and patient survival after pancreatic resections for underlying malignancy over a 20-year observation period in a European high-volume cancer center.
Methods
Patient inclusion criteria
This was a retrospective single-center analysis conducted in a tertiary referral center for pancreatic surgery. All patients undergoing pancreatic resections with underlying malignancy between March 1989 and May 2017 were entered into a prospective database. The patients were classified into four groups according to their BMI (kg/m2); group 1 (underweight) <18.5 kg/m2, group 2 (normal weight), 18.5–25.0 kg/m2, group 3 (overweight) 25.1–30.0 kg/m2, group 4 (obese) >30.0 kg/m2. Approval was granted by an independent ethics committee. Patient characteristics were extracted from our medical records and further analyzed.
Preoperative assessment
Patients were assessed preoperatively by medical history, physical examination and laboratory evaluation. Computed tomography (CT) or magnetic resonance imaging were used preoperatively to evaluate local tumor dimensions and detect distant metastases. All indications for resections were endorsed in an interdisciplinary consensus meeting. For tumor staging, the 7th edition of the American Joint Committee on Cancer/Union for International Cancer Control (UICC) staging system was applied (16).
Surgical procedure
All included operations were performed in an open surgical technique according to international standards at that time. After laparotomy, peritoneal metastases were initially excluded by complete exploration of the abdominal cavity. Access to the omental bursa was established by dissection of the gastrocolic ligament. After retraction of the stomach and inspection of the pancreas, local resectability and the extent of the resection were determined based on local findings. Dissection of the pancreas was done by either electrocautery or scalpel. A standard lymphadenectomy was performed. Pancreatoenteral anastomosis was performed as either pancreatojejunostomy or a pancreatogastrostomy depending on the individual surgeon’s preference. Every patient received at least one intra-abdominal drain (Degania Silicone Europe GmbH, Regensburg, Germany) to measure postoperative amylase levels and drain output in the postoperative course.
Postoperative management
Postoperative care was standardized. All patients were monitored for at least one day at a specialized surgical intensive care unit (ICU). Amylase levels were examined in the serum and in the intraoperatively placed abdominal drains on the second postoperative day and every patient received a nasogastric tube for gastric decompression. In the absence of signs of a pancreatic fistula, oral food intake was started depending on the clinical presentation and tolerance. The concept of enhanced recovery after surgery (ERAS) has not been applied within the study period. Every complication within 90 days postoperative was defined as postoperative morbidity and every death within the first 30 postoperative days was defined as postoperative mortality. The 90-Day mortality rate was also reported. Using the Dindo-Clavien classification, major postoperative complications were graded as complications requiring surgical, endoscopic, or radiologic intervention (grade III); life-threatening complications requiring intensive care management (grade IV), and death (grade V) (17), All resected specimens were histologically analyzed by specialized pathologists to evaluate tumor stage, grading, lymph node status, and resection margins. The 7th edition of the TNM classification was used. R0 was defined as neither macroscopic nor microscopic tumor cells detectable in postoperative pathology. R1 was defined as microscopic tumor cells detected in pathology and R2 was defined as macroscopic remaining tumor seen either intraoperatively or in pathology. The diagnosis of a postoperative pancreatic fistula formation (POPF) was based on the definition of the International Study Group on Pancreatic Fistula (ISGPF) (18). Postpancreatectomy hemorrhage (PPH) was also defined based on the International Study Group of Pancreatic Surgery (ISGPS) definitions (19).
Statistics
The data were collected in a database (Microsoft Access 2.0, Microsoft Corporation, Seattle, USA) and evaluated retrospectively. Unless otherwise specified, the data are expressed as mean. Student’s t-test and ANOVA were used to compare means of quantitative variables as appropriate. Categorical data were compared using chi-square tests as appropriate. Survival analysis was determined by means of the Kaplan-Meier method and multivariate analysis was performed by the Cox proportional hazards model and Logistic regression where appropriate using Stata for Windows 14.0 (Stata Corporation, College Station, TX, USA). Multivariable hazard ratios (HRs) and 95% confidence intervals were calculated using Cox proportional hazards regression models. A P value below 0.05 was considered significant.
Results
Patient characteristics
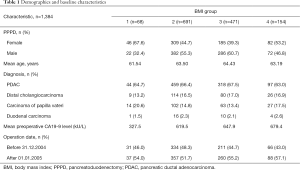
Between 1989 and 2017, 1,384 patients underwent pancreatic resections for histologically verified underlying malignancy at our institution. Histologically, the study includes 918 patients with adenocarcinoma of the pancreas (66.3%), 229 patients with distal cholangiocarcinoma (16.5%), 206 ampullary carcinoma patients (14.9%), and 31 duodenal carcinoma patients (2.2%). Of these patients, 762 (55.1%) were men and 622 (44.9%) were women, with a median age of 63.7 [18–93] years at the time of operation. The median BMI in the patient group was 24.8 (16.1–53.0) kg/m2; 25.0 for men and 24.7 for women. The patients were classified into four groups according to their BMI (kg/m2); group 1 (underweight) <18.5 kg/m2, group 2 (normal weight), 18.5–25.0 kg/m2, group 3 (overweight) 25.1–30.0 kg/m2, group 4 (obese) >30.0 kg/m2. Group 1 consisted of 68 patients (4.9%), group 2 of 691 patients (50.0%), group 3 of 471 patients (34.0%) and group 4 of 154 patients (11.1%). Preoperative laboratory chemical examinations gave a mean CA 19-9 value of 621 kU/L median 104.00 U/L; range, 0–10,832 kU/L) (Table 1).
Full table
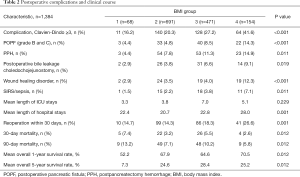
Postoperative characteristics and surgical complications
The mean length of hospital stay was 23.0 [2–356] days. The mean stay in the ICU was 5.11 [1–127] with a duration of 5.1 [1–127] days and 5.1 [1-124] days for men and women, respectively. Postoperative complications were observed in 343 (24.8%) of cases. PPH occurred in 133 patients (9.6%), 98 (7.1%) patients developed clinically relevant POPF grade B and C, wound infection developed in 64 patients (4.6%), SIRS/Sepsis occurred in 45 cases (3.3%), while 73 patients developed an insufficiency of the hepaticojejunostomy (5.3%). The perioperative 30-day mortality was 4.8%, in this period a total of 124 patients died. A total of 226 patients died within 90 days postoperatively resulting in a postoperative 90-day mortality of 12.3%. Within a mean observation period of 687.7 [2–8,500] days, 735 (53.1%) patients died [40 in group 1 (58.8%), 375 in group 2 (54.2%), 243 in group 3 (51.6%) and 77 (50.0%) in group 4] (Table 2).
Full table
Postoperative morbidity and mortality pertaining to BMI
There were important differences in postoperative complications (group 1, 16.2%; group 2, 20.3%; group 3, 27.2%; group 4, 41.6%) with the type of postoperative complications also varying between the groups as illustrated in Table 2. PPH occurred more in obese patients (14.9%) compared to 7.8% of patients with a normal BMI (18.5–20). POPF occurred significantly more in obese patients (14.3%) compared to 4.8% of patients with normal BMI (P=0.001) Insufficiency of the hepaticojejunostomy was found in 9.1% of patients in group 4 and 3.8% of patients in group 2 (P=0.011). While 12.3% of obese patients also had wound infection, only 3.5% of patients with a normal BMI did (P=0.001). SIRS/Sepsis occurred more often in obese patients (7.1%) compared to 2.2% of non-obese patients. In total, 26.6% of obese patients required reoperation due to complications while only 14.3% of patients with a BMI in the normal range required reoperation. The overall length of postoperative hospital stays, as well as the total time spent in the ICU, reflected this pattern (Table 2). Underweight patients showed a higher perioperative mortality compared to patients with normal BMI (7.7% vs. 3.9%, P=0.012. The lowest 30-day mortality rate was seen in group 4 (3.1%). Similarly, the lowest 90-day mortality rate was seen in group 2 (7.9%), followed by group 4 (10.2%) and group 3 (11.5%) with group 1 having the highest mortality rate (14.3%).
Long-term survival
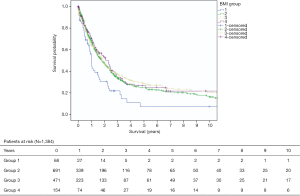
After a median follow-up time of 20.7 [0–279] months, the overall 1-, 5-, 10- and 15-year survival rates were 66.4%, 25.5%, 17.9%, and 12.1%, respectively. The survival rates varied amongst the four BMI groups as seen in Table 2. For patients in BMI group 1 the 1-, 5-year survival rates were 52.2% and 7.3% respectively, in BMI group 2 the 1-, 5-year survival rate was 67.9% and 24.6% respectively, in BMI group 3 the 1-, 5-year survival rates were 64.6% and 28.4% and in BMI group 4 the 1-, 5-year survival rates were 70.5% and 25.2% (Figure 1).
Histopathology
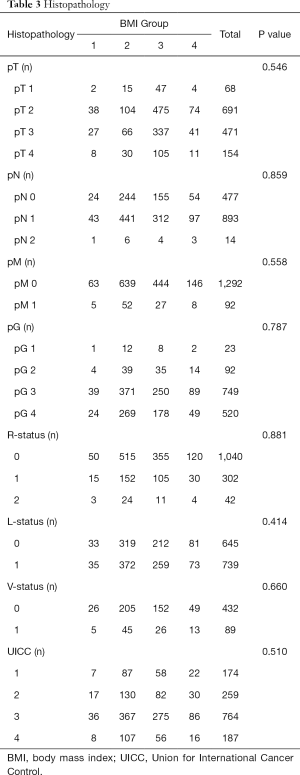
In 1,040 (75.1%) patients an R0 resection was achieved, R1 resection and R2 resection were achieved in 302 (21.8%) and 42 (3.0%) patients, respectively. As a result of classifying the 1,384 patients as per the UICC stages, 174 (12.6%) patients were stage 1 and 259 (18.7%) patients were stage 2. Stage 3, with 764 patients (55.2%), was the most frequent. A total of 187 patients (13.5%) were classified as stage 4. No significantly different characteristics for tumor stage (P=0.546), lymph node stage (P=0.859), UICC stage (P=0.510), lymphangiosis carcinomatosa (P=0.414), venous invasion (P=0.660), positive resection margins (P=0.881), or histologic tumor differentiation (P=0.787) could be seen amongst patients in the 4 BMI groups (Table 3).
Full table
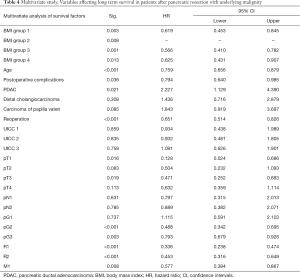
Predictors of overall survival (OS)
Detailed analysis of predictors of OS in obese as well as underweight patients are presented in Table 4. BMI <18.5 (P=0.012) Postoperative complications (P≤0.001), age > 65 (P=0.003), T status (P≤0.001), reoperation (P≥0.001), lymph node stage (P≤0.001), UICC score (P≤0.001), diagnosis group (P≤0.001), M status (P≤0.001), G status (P≤0.001), and positive resection margins (R1/R2; P≤0.001) were significantly associated with worse OS in univariate analysis. In multivariate analysis, age >65 [HR 0.759; 95% confidence interval (CI): 0.656–0.879; P≤0.001] postoperative complications (HR 0.794; 95% CI: 0.640–0.985; P=0.036) and BMI <18.5 (HR 0.619; 95% CI: 0.453–0.845; P=0.003), PDAC (HR 2.227; 95% CI: 1.129–4.390; P=0.021), reoperation (HR 0.651; 95% CI: 0.514–0.826; <0.001), as well as M status (HR 0.577; 95% CI: 0.384–0.867; P=0.008) positive resection margin (R1 <0.001; HR 0.336; 95% CI: 0.238–0.474 and R2 <0.001; HR 0.453; 95% CI: 0.316–0.649) and T status (pT3; P=0.019, HR 0.471; 95% CI: 0.252–0.883) were independently associated with OS in patients.
Full table
Discussion
Obesity is considered a risk factor for a higher morbidity and mortality in hospitalized surgical patients (20) and has been increasingly recognized as a relevant risk factor of pancreatic cancer. While some epidemiological and clinical studies have shown that obesity is associated with increased incidence of pancreatic cancer and potentially worse cancer outcome, there is no clear consensus on the impact of body mass on hospital morbidity and mortality and long-term survival especially in patients undergoing pancreatic surgery for underlying malignancy. Survival benefits for overweight and obese patients, compared to normal or underweight patients have been reported, especially in postoperative ventilator-induced lung injury or sepsis, this effect is defined as the ‘obesity paradox’. Mullen et al. (15) proposed the existence of an obesity paradox in the general surgery patient population by analyzing data on patients undergoing non-bariatric general surgery and reported a lower perioperative mortality for overweight and moderately obese patients. Valentijn et al. (7) reviewed existing literature on the obesity paradox in the surgical population, showing worst mortality rates for underweight and morbidly obese patients and concluding that the etiology of the obesity paradox is multifactorial. They speculated that overweight and mildly obese patients might have more sufficient nutritional reserves than their underweight or obese counterparts leading to a more appropriate inflammatory and immune response to the surgical stress. Contrastingly, hyperinsulinism and high levels of blood-activated insulin-like growth factor 1 (IGF-1) result from insulin resistance associated with lifestyle-related diseases can contribute to tumor promotion through the resultant activation of cell proliferation, apoptosis, and angiogenesis as demonstrated by Louie et al. (5). Despite these diverging theories, there have been only few reports regarding the influence of body weight on the prognosis of periampullary cancer, and the findings from these studies have been controversial. In this large-scale study, we analyzed the effect of preoperative body weight on outcomes following pancreatic resections in patients with underlying malignancy in a tertiary referral center for pancreatic surgery and indicated that obese patients have a higher likelihood of experiencing postoperative complications. However, long-term survival remained unaffected. Obese patients in our study showed higher postoperative morbidity rates and length of hospital stay (mainly due to increased incidence of pneumonia and wound infections), and higher mortality rates compared to non-obese patients. However, while long-term outcomes did not significantly differ between the BMI groups 2–4, possibly due to comparable UICC stages in all groups, patients in group 1 showed a significantly reduced long-term survival when compared to the other BMI-groups (P=0.023). Our findings are consistent with similar studies reported in the literature. Lachmann et al. observed the factors affecting the downregulation of mHLA-DR as a general biomarker of impaired immunity seen in patients with sepsis and pneumonia and after major surgery (21). They further showed that overweight is a risk factor for an impaired immunity after surgery and therefore coincides with an increased risk for postoperative complications. Our data support these findings, as we found an increase in postoperative morbidity in obese patients that resulted mainly from a significantly higher incidence of pneumonia and a higher trend toward intraabdominal infections, postoperative bleedings and wound infection rates. Amodu et al. also showed that a higher BMI increases the risk for postoperative complications after pancreatectomy (22). Our data is further supported by a study on the impact of obesity on surgical and oncologic outcomes by Del Chiaro et al., who found that low BMI was associated with a decreased long-term survival. However, their multivariate analysis of 367 patients undergoing resection for pancreatic adenocarcinoma could not identify obesity as an independent risk factor for postoperative complications (23,24). The findings from these studies have however been controversial. In an analysis of 841 patients with pancreatic adenocarcinoma Li et al. found that overweight or obesity during early adulthood was associated with a greater risk of pancreatic cancer and a younger age of disease onset and obesity at an older age was associated with a lower overall survival in patients with pancreatic cancer (25). Yuan et al. and Kasenda et al. found that higher prediagnostic BMI was associated with decreased long-term survival (9,26). Recently, Shi et al. published a meta-analysis quantifying the association between BMI and OS of pancreatic cancer. Their analysis showed that obesity in adulthood shortened OS of pancreatic cancer patients (HR 1.29, 95% CI: 1.17–1.41) (8). In contrast with our own data, which suggested OS remained unaffected by obesity.
The strengths of our study include a large data set and data analysis from a high-volume cancer center in a retrospectively collected, externally validated, internally audited clinical database. The database included pancreatectomy-specific outcomes, such as 30- and 90-day mortality, POPF, and PPH. The respective details necessary for pathologic and radiologic correlations were also compiled. There are weaknesses, however, in our study. The tentative association between BMI and cancer survival is likely to be explained by several methodologic limitations including confounding, reverse causation, and collider-stratification bias. The inadequacy of BMI as a measure of adipose tissue in cancer patients is in its limited ability to adequately reflect body composition. The use of retrospective data analysis is also dependent on appropriate coding and interpretation of clinical events. Missing data is also an issue that inevitably decreases statistical power and may introduce bias. In our present study, missing variables for the covariates of cardiac disease, vascular disease, and ethanol use introduced collinearity into our models, such that we had to exclude some of these variables in our multivariable models. These missing variables may have affected the integrity of our models, although our c-statistic scores suggest adequate predictive ability. Furthermore, there was a lack of surgical data, such as blood loss, anesthesia time, and operative time. In our study, our patients tended to have lower tumor stages and a larger resection margin in obese patients, although these differences were not statistically significant. This could explain why we found a higher postoperative mortality in obese patients compared to patients with a normal BMI, but comparable long-term survival rates for the two groups. Moreover, physicians may consider obese patients at higher risk of a worse outcome potentially resulting in earlier admission to the ICU for monitoring purposes as well as increased use of prophylactic measures including mobilization, stricter glycaemic control, and stricter mechanical ventilation parameters. Other factors contributing to the divergent results in literature are significant heterogeneity in study design and method (e.g., study population, follow-up length, varying BMI groups); time of BMI assessment (pre-, peri-, or post-diagnosis); and lack of consideration for variability in the strength and directions of associations by age, sex, race/ethnicity, and cancer subtype.
Conclusions
In contrast to the convincing evidence that obesity (measured by BMI) increases the risk of many different types of cancer, the role of obesity in survival among cancer patients remains ambiguous. Some studies suggest that higher BMI decreased mortality risk in cancer patients, a phenomenon called the obesity paradox. Our retrospective analysis of 1,384 patients who underwent resection for pancreatic cancer does not support the obesity paradox. In our study, obesity was associated with a longer length of stay, and higher postoperative morbidity and mortality. Interestingly, 5-year OS rates were however slightly higher in obese and overweight patients. Although BMI may be too simple to evaluate sophisticated interactions between different body fat compartments and inflammatory and immune responses, reliable but practical methods to quantify body fatness, composition, and weight trajectories accurately in cancer survivors are needed to advance this emerging field and to develop guidelines for the integration of BMI-status into our daily clinical practice.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Approval was granted by an independent ethics committee (Approval ID: EA2/035/14).
References
- Rahib L, Smith BD, Aizenberg R, et al. Projecting Cancer Incidence and Deaths to 2030: The Unexpected Burden of Thyroid, Liver, and Pancreas Cancers in the United States. Cancer Res 2014;74:2913-21. [Crossref] [PubMed]
- Vincent A, Herman J, Schulick R, et al. Pancreatic cancer. Lancet 2011;378:607-20. [Crossref] [PubMed]
- Chari ST, Kelly K, Hollingsworth MA, et al. Early Detection of Sporadic Pancreatic Cancer: Summative Review. Pancreas 2015;44:693-712. [Crossref] [PubMed]
- Midha S, Chawla S, Garg PK. Modifiable and non-modifiable risk factors for pancreatic cancer: A review. Cancer Lett 2016;381:269-77. [Crossref] [PubMed]
- Louie SM, Roberts LS, Nomura DK. Mechanisms linking obesity and cancer. Biochim Biophys Acta 2013;1831:1499-508. [Crossref] [PubMed]
- Nogueira L, Stolzenberg-Solomon R, Gamborg M, et al. Childhood Body Mass Index and Risk of Adult Pancreatic Cancer. Curr Dev Nutr 2017. [Crossref] [PubMed]
- Valentijn TM, Galal W, Hoeks SE, et al. Impact of Obesity on Postoperative and Long-term Outcomes in a General Surgery Population: A Retrospective Cohort Study. World J Surg 2013;37:2561-8. [Crossref] [PubMed]
- Shi YQ, Yang J, Du P, et al. Effect of Body Mass Index on Overall Survival of Pancreatic Cancer: A Meta-Analysis. Medicine (Baltimore) 2016;95:e3305. [Crossref] [PubMed]
- Yuan C, Bao Y, Wu C, et al. Prediagnostic Body Mass Index and Pancreatic Cancer Survival. J Clin Oncol 2013;31:4229-34. [Crossref] [PubMed]
- Lu Y, Hajifathalian K, Ezzati M, et al. Metabolic mediators of the effects of body-mass index, overweight, and obesity on coronary heart disease and stroke: a pooled analysis of 97 prospective cohorts with 1·8 million participants. Lancet 2014;383:970-83. [Crossref] [PubMed]
- Abarca-Gómez L, Abdeen ZA, Hamid ZA, et al. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet 2017;390:2627-42. [Crossref] [PubMed]
- Arabi YM, Dara SI, Tamim HM, et al. Clinical characteristics, sepsis interventions and outcomes in the obese patients with septic shock: an international multicenter cohort study. Crit Care 2013;17:R72. [Crossref] [PubMed]
- Ball L, Serpa Neto A, Pelosi PJ. Obesity and survival in critically ill patients with acute respiratory distress syndrome: a paradox within the paradox. Crit Care 2017;21:114. [Crossref] [PubMed]
- Klein F, Jacob D, Bahra M, et al. Prognostic factors for long-term survival in patients with ampullary carcinoma: the results of a 15-year observation period after pancreaticoduodenectomy. HPB Surg 2014;2014:970234. [Crossref] [PubMed]
- Mullen JT, Moorman DW, Davenport DL. The obesity paradox: body mass index and outcomes in patients undergoing nonbariatric general surgery. Ann Surg 2009;250:166-72. [Crossref] [PubMed]
- Sobin L, Gospodarowicz M, Wittekind, C. TNM classification of malignant tumours-7th ed. Chichester: Wiley-Blackwell, 2009.
- Clavien PA, Barkun J, de Oliveira ML, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 2009;250:187-96. [Crossref] [PubMed]
- Bassi C, Butturini G, Molinari E, et al. Pancreatic fistula rate after pancreatic resection. The importance of definitions. Dig Surg 2004;21:54-9. [Crossref] [PubMed]
- Wente MN, Veit JA, Bassi C, et al. Postpancreatectomy hemorrhage (PPH): an International Study Group of Pancreatic Surgery (ISGPS) definition. Surgery 2007;142:20-5. [Crossref] [PubMed]
- Tjeertes EK, Hoeks SE, Beks SB, et al. Obesity--a risk factor for postoperative complications in general surgery? BMC Anesthesiol 2015;15:112. [Crossref] [PubMed]
- Lachmann G, Kurth J, Haefen C, et al. In vivo application of Granulocyte-Macrophage Colony-stimulating Factor enhances postoperative qualitative monocytic function. Int J Med Sci 2017;14:367-75. [Crossref] [PubMed]
- Amodu L, Alexis J, Soleiman A, et al. Body mass index and post-operative complications predict early readmission in patients undergoing pancreatic surgery: a retrospective review of 383 cases. HPB 2017;19:S172-3. [Crossref]
- Del Chiaro M, Rangelova E, Ansorge C, et al. Impact of body mass index for patients undergoing pancreaticoduodenectomy. World J Gastrointest Pathophysiol 2013;4:37-42. [Crossref] [PubMed]
- Jiang QL, Wang CF, Tian YT, et al. Body mass index does not affect the survival of pancreatic cancer patients. World J Gastroenterol 2017;23:6287-93. [Crossref] [PubMed]
- Li D, Morris JS, Liu J, et al. Body Mass Index and Risk, Age of Onset, and Survival in Patients With Pancreatic Cancer. JAMA 2009;301:2553-62. [Crossref] [PubMed]
- Kasenda B, Bass A, Koeberle D, et al. Survival in overweight patients with advanced pancreatic carcinoma: a multicentre cohort study. BMC Cancer 2014;14:728. [Crossref] [PubMed]


