Liver hilar abscesses secondary to gastrointestinal perforation by ingested fish bones: surgical management of two cases
Introduction
Fish bones are the most common foreign bodies ingested accidentally during adulthood (1). These ingested foreign bodies are associated with the highest risk of gastrointestinal perforation, especially when their ends are thin and sharp (2,3). In addition to a nonspecific clinical presentation, most patients do not remember the fish bone ingestion, making the diagnosis difficult due to the delay between ingestion and symptoms (2,3).
Several hepatobiliary complications secondary to gastrointestinal perforation after ingestion of a fish bone have been described in the literature, the most common being liver abscess, which can be potentially fatal (4-6). Treatment involves removal of the foreign body if possible (endoscopically or surgically), drainage of the abscess (radiologically or surgically), and appropriate antibiotic therapy (4,7).
To our knowledge, no cases of hepatic hilar abscesses secondary to gastrointestinal perforation by a fish bone have been described in the literature. We report surgical management of two cases of abscess localized in the hepatic hilum secondary to the ingestion of fish bones.
Case reports
Case 1
A 63-year-old woman who had history of hypothyroidism and hypercholesterolemia was admitted to our department for a progressive increasing epigastric abdominal pain with fever for 10 days. Physical examination revealed a fever of 38.5 °C, a soft abdomen and tenderness in the epigastric and right upper quadrant regions with no palpable mass.
Laboratory tests revealed leukocytosis of 12.6 G/L with neutrophilia of 9.8 G/L. C-reactive protein increased to 74.9 mg/L and alkaline phosphatase was 147 IU/L. Lipase, aminotransferases, GGT, bilirubin, and the rest of the biological tests were within normal limits.
Hepatic ultrasonography showed a hypoechoic lesion in the hepatic hilum containing a hyperechoic linear structure at its center. Contrast-enhanced CT scan confirmed the presence of a heterogeneous tissue mass of 3.6 cm ×2.5 cm (Figure 1A), between segment I of the liver and portal vein at the level of the hepatic hilum in close contact with the hepatic artery (Figure 1B). Within this mass, a hyperdense linear structure was seen, suggesting the diagnosis of migration after gastrointestinal perforation by an ingested foreign body (Figure 1). The subsequent anamnesis of the patient did not confirm fish bone ingestion.
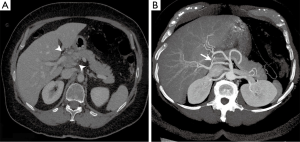
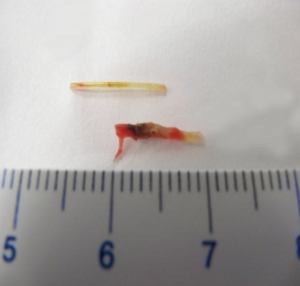
The indication for laparotomy was retained and exploration of the hepatic pedicle highlighted an abscess of 40 mm ×30 mm from the liver hilum to the pancreas head. A 4-cm fish bone was isolated within granulation tissue (Figure 2). Otherwise, gastric and duodenal wall explorations did not show evidence of perforation. The fish bone was removed and the abscess drained. The postoperative course was uneventful. Abdominal contrast-enhanced CT scan was performed at day 7 and the improvement in clinical state allowed the patient leave our hospital at day 8. The contrast-enhanced abdominal CT scan at 6 months showed no abnormality or secondary complication, and the patient did not report abdominal symptoms.
Case 2
An 83-year-old woman, otherwise healthy, was admitted to our department for management of acute intestinal obstruction. Physical examination revealed a fever of 39 °C, a distended abdomen, diffuse abdominal pain, and tenderness in the right upper quadrant and epigastric regions at palpation with localized defense without contracture.
Laboratory tests showed leukocytosis of 17 G/L, creatinine of 130 µmol/L, and C-reactive protein levels of 400 mg/L. Abdominal contrast-enhanced CT scan required in emergency brought to light a linear hyperdense foreign body inside an abscess of the hepatic hilum extended to hepatic segment III (Figure 3). There was also a pneumoperitoneum and perihepatic and periduodenal collections. The subsequent anamnesis confirmed that the patient had eaten fish 4 days before.

The indication for laparotomy was decided. After washing and draining perihepatic periduodenal collections, fish bone removal and liver abscess drainage were performed. A feeding jejunostomy was performed. The patient had an uneventful postoperative course. Abdominal contrast-enhanced CT scan performed at day 7 and clinical improvement allowed the patient to be discharged at day 9. Closure of the jejunostomy was performed at day 45 and recovery of oral feeding was allowed. The abdominal contrast-enhanced CT scan at 6 months did not show any abnormalities or complications, and the patient did not report any somatic abdominal complaint.
Discussion
Accidental ingestion of foreign bodies is a common clinical situation, especially in children or elderly patients with cognitive disorders, swallowing disorders or oral and dental alterations (1,2,8,9). In most cases, ingested foreign bodies are asymptomatic and pass through the gastrointestinal tract uneventfully within 1 week (2,9-11).
Gastrointestinal complications due to perforations usually occur when the foreign body is sharp or pointed (fish bones, chicken bones, toothpicks, etc.) and seem favored by a preexisting anatomical abnormality of the digestive tract (inflammatory bowel disease, bowel tumor, diverticular disease, etc.) (2,10,12). Perforation can occur at any site of the gastrointestinal tract, but the ileocecal and rectosigmoid regions appear to be the most commonly affected (2,10). Among the various foreign bodies ingested, the fish bone is not only the most commonly encountered (especially in Asian countries where fish consumption is very common), but it is also one that presents a significant risk of gastrointestinal perforation requiring surgical exploration (8,12).
Numerous reports of ingestion of fish bones penetrating the aerodigestive tract and migrating to various parts of the chest or abdominal cavity have been reported. These may be responsible for various complications, which are most frequently represented by infectious complications: retropharyngeal, epidural, brain, pancreatic, hepatic, or perivesical abscesses; mediastinitis; and empyema (1,10,13-15).
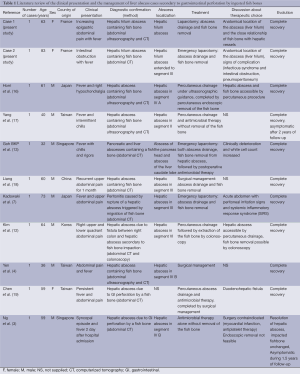
Hepatobiliary complications secondary to gastrointestinal perforation by ingested fish bones are relatively rare. Liver abscess seems to represent the hepatobiliary complication secondary to fish bone migration in the hepatic region that is the most frequently reported in the literature (Table 1) (3,4,7,12,16-19). Few exceptional cases of symptomatic biliary tract lithiases secondary to the presence of asymptomatic fish bones serving as a nidus for stone formation in the common bile duct have been described (10,20,21). A case of cholecystitis secondary to migration of a fish bone through the gastrointestinal tract has also been reported (11).
Full table
In our cases, only one patient remembered eating fish 4 days before and they did not remember the accidental ingestion of a fish bone. In this case, the onset of complications (reflex ileus and localized peritoneal irritation) appeared very quickly, only 4 days after ingestion. In the second case, the patient did not remember ingesting a foreign body. Moreover, the per-operative exploration of duodenal and gastric walls did not show any signs of perforation, suggesting a significant delay between ingestion of the foreign body and the occurrence of symptoms.
Indeed, only a very small number of patients remember the ingestion of a foreign body. Furthermore, the time of symptom onset, ranging from 2 weeks to 1 year from ingestion, makes the anamnestic diagnosis clearly more difficult (1,2).
In case of hepatobiliary complications, abdominal X-ray is irrelevant and does not lead to the diagnosis when there is fish bone ingestion, because it is radiolucent (2,10). However, abdominal sonography was used to guide diagnosis objectifying, in case 1 the hepatic abscess. Abdominal contrast-enhanced CT scan with secondary reformatted images allowed us to confirm the diagnosis in our two cases, which is consistent with data found in the literature (3,7,10,14,22). Abdominal CT scan was also used to visualize the extent of the lesions, eliminate differential diagnoses, and retain the indication for surgery in both cases.
The optimal management of foreign body ingestion is widely debated in the literature. Velitchkov NG et al. [1996] proposed an algorithm for the management of ingested foreign bodies. In most cases, it seems reasonable to assume that accidental ingestion of an asymptomatic foreign body requires only simple monitoring (9). It is clear that the properties of the foreign body determine the risk of perforation. Obviously, thin and sharp objects such as fish bone should be considered at risk of further complications because they have a high risk of perforation. Ngan JH et al. [1990] recommend a flexible endoscopy for all patients complaining of fish bone ingestion because of potential secondary complications (8,9). When oral cavity examination does not allow detection of fish bones and furthermore, its removal, flexible endoscopy is required under local anesthesia and will be guided by the painful symptoms reported by the patient, which helps to determine the precise location of the fish bone, allowing its removal with forceps in most cases (8). However, when the perforation occurs and the patient becomes symptomatic with signs of peritonitis, intestinal obstruction or gastrointestinal bleeding, the data in the literature clearly document the indication for surgery (Table 1) (1,7,9,12). Moreover, in rare cases, liver abscess secondary to gastrointestinal perforation by a fish bone can be fatal when secondary sepsis occurs (5,6).
For these two cases, indication for surgical treatment by laparotomy was decided because of the liver hilum location of the abscesses and the close relationship of fish bones with hepatic vessels, and also because of the signs of complications revealed by clinical examination or complementary examination such as blood test or imaging data, such as infectious syndrome, peritonitis, reflex ileus, or pneumoperitoneum. Indeed, medical treatment by antibiotics alone and/or radiological treatment by transhepatic percutaneous drainage for the management of liver abscesses secondary to the migration of fish bones have already been reported in the literature in patients whose surgery is contraindicated or not (Table 1) (3,4,12,16,17). However, surgical treatment with removal of the fish bone and abscess drainage seems to be the reasonable therapeutic option to choose, a fortiori in cases where liver abscesses present an inaccessible anatomical location to percutaneous drainage or present a high risk of vascular damage, such as hepatic hilar regions or the hepatic pedicle. This surgical management may be chosen for patients with clinical, biological, or radiological signs of severity that suggest gastrointestinal perforation: peritonitis associated with an infectious syndrome whose evolution could be potentially fatal.
Acknowledgements
We thank Emmanuel Schaeffer and Jocelyne Wuibout for the proofreading and the correction of this manuscript.
Disclosure: The authors declare no conflict of interest.
References
- Symeonidis D, Koukoulis G, Baloyiannis I, et al. Ingested fish bone: an unusual mechanism of duodenal perforation and pancreatic trauma. Case Reports Gastrointest Med 2012;2012:308510.
- McCanse DE, Kurchin A, Hinshaw JR. Gastrointestinal foreign bodies. Am J Surg 1981;142:335-7. [PubMed]
- Ng CT, Htoo A, Tan SY. Fish bone-induced hepatic abscess: medical treatment. Singapore Med J 2011;52:e56. [PubMed]
- Yen HH, Hsu YC. Gastrointestinal-pyogenic liver abscess associated with a penetrating fish bone. J Gastroenterol Hepatol 2010;25:1900. [PubMed]
- de la Vega M, Rivero JC, Ruíz L, et al. A fish bone in the liver. Lancet 2001;358:982. [PubMed]
- Theodoropoulou A, Roussomoustakaki M, Michalodimitrakis MN, et al. Fatal abscess caused by a fish bone. Lancet 2002;359:977. [PubMed]
- Kadowaki Y, Tamura R, Okamoto T, et al. Ruptured hepatic abscess caused by fish bone penetration of the duodenal wall: report of a case. Surg Today 2007;37:1018-21. [PubMed]
- Ngan JH, Fok PJ, Lai EC, et al. A prospective study on fish bone ingestion. Experience of 358 patients. Ann Surg 1990;211:459-62. [PubMed]
- Velitchkov NG, Grigorov GI, Losanoff JE, et al. Ingested foreign bodies of the gastrointestinal tract: retrospective analysis of 542 cases. World J Surg 1996;20:1001-5. [PubMed]
- Kim YH, Kim YJ, Park WK, et al. Fish bone as a nidus for stone formation in the common bile duct: report of two cases. Korean J Radiol 2004;5:210-213. [PubMed]
- Kunizaki M, Kusano H, Azuma K, et al. Cholecystitis caused by a fish bone. Am J Surg 2009;198:e20-2. [PubMed]
- Kim YM, Lee TH, Jung SH, et al. Hepatic abscess that formed secondary to fish bone and had fistula with the ascending colon. Dig Dis Sci 2007;52:3515-8. [PubMed]
- Goh BK, Yong WS, Yeo AW. Pancreatic and hepatic abscess secondary to fish bone perforation of the duodenum. Dig Dis Sci 2005;50:1103-6. [PubMed]
- Wang WL, Liu KL, Wang HP. Clinical challenges and images in GI. Pancreatic abscess resulting from a fish bone penetration of the stomach. Gastroenterology 2008;135:1865. [PubMed]
- Maramattom BV, Thomas B, Kerala DK. Epidural and brain abscess following pearl spot fish bone injury. Neurology 2012;79:484-5. [PubMed]
- Horii K, Yamazaki O, Matsuyama M, et al. Successful treatment of a hepatic abscess that formed secondary to fish bone penetration by percutaneous transhepatic removal of the foreign body: report of a case. Surg Today 1999;29:922-6. [PubMed]
- Yang CY, Kao JH, Liu KL, et al. Medical treatment of fish bone-related liver abscess. Clin Infect Dis 2005;41:1689-90. [PubMed]
- Liang H, Liu OQ, Ai XB, et al. Recurrent upper quadrant pain: a fish bone secondary to gastric perforation and liver abscess. Case Rep Gastroenterol 2011;5:663-6. [PubMed]
- Chen HK, Kuo JR, Uen YH, et al. Liver abscess secondary to fish bone migration from the duodenum. ANZ J Surg 2011;81:206. [PubMed]
- Procházka V, Krausová D, Kod’ousek R, et al. Foreign material as a cause of choledocholithiasis. Endoscopy 1999;31:383-5. [PubMed]
- Kaji H, Asano N, Tamura H, Yuh I. Common bile duct stone caused by a fish bone: report of a case. Surg Today 2004;34:268-71. [PubMed]
- Lue AJ, Fang WD, Manolidis S. Use of plain radiography and computed tomography to identified fish bone foreign bodies. Otolaryngol Head Neck Surg 2000;123:435-8. [PubMed]