Liver transplantation in a patient with complex anomaly of the inferior vena cava
Introduction
The embryogenesis of the inferior vena cava (IVC) is a complex process involving the formation of several anastomoses between embryonic veins (1,2). Since the introduction of noninvasive imaging exams such as computed tomography and magnetic resonance, congenital anomalies of the IVC have become more commonly recognized (3,4). More than one anomaly can coexist on a single patient (5).
Zinser and Hanto described in 2012 the first successful orthotopic liver transplantation (OLT) in an asymptomatic adult with an interrupted IVC and azygos continuation (6). Hatipoglu et al. reported a living donor liver transplantation in a patient with IVC absence (7). Liver transplantation has also been performed in patients with other IVC anomalies, such as left-sided extrahepatic IVC (8). We describe herein the first successful report of an OLT in an asymptomatic adult with complex IVC anomaly: duplication of the infrarenal IVC, azygos continuation of the IVC, agenesia of the hepatic portion of the IVC and presence of several anomalous veins communicating the common iliac vein and the IVC of one side with the contralateral side.
Case report
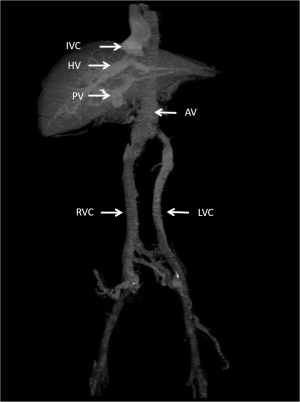
A 57-year-old white male with a 4.8 cm hepatocellular carcinoma and advanced chronic liver disease secondary to hepatitis C virus was referred to our hospital for liver transplantation. Laboratories exams were hemoglobin 10.2 g/dL, leukocytes 1.800/mm3, platelets 69.000/mm3, creatinine 0.9 mg/dL, total bilirubin 0.8 mg/dL, alanine aminotransferase 48 U/L, albumin 3.8 g/dL, and alpha-fetoprotein 48 ng/mL. A CT of the thorax showed severe dilation of the azygos vein mimicking IVC thrombosis. A venous abdominal angio CT with infusion of contrast material into a dorsal vein of both feet showed duplication of the IVC from the confluence of the external with the internal iliac veins up to 1cm above the renal veins. Both the right and left IVC ascended cranially along the respective side of the abdominal aorta (Figure 1). After receiving blood from the respective renal veins, both IVC joined at the level of the lower face of the twelfth thoracic vertebra and passed posterior to the diaphragmatic crura to enter the thorax as the azygos vein. A very proeminent azygos vein joined the superior vena cava at the normal location in the right paratracheal area. The retrohepatic segment of the IVC was absent. The hepatic veins drained into a short suprahepatic portion of the IVC. There were also several anomalous veins of 0.8 to 1.2 cm in diameter that drained blood from one side of the common iliac vein and the IVC into the respective veins of the contralateral side.
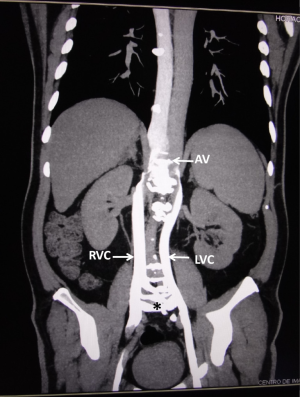
A liver from a deceased donor was procured. At the time of transplantation, the short suprahepatic portion of the IVC was identified and clamped. The right, middle, and left hepatic veins were sectioned and joined in a single, wide cuff, using venoplasty. This single orifice was anastomosed to the suprahepatic IVC of the new liver. The retrohepatic donor vena cava stump was closed with running suture (piggy-back technique). The portal vein, hepatic artery, and common duct were anastomosed termino-terminal as usual. No venovenous bypass was used. The operative time was 260 minutes with a warm ischemia time of 55 minutes. No blood transfusions were given. The patient had an uncomplicated postoperative course and was discharged on postoperative day 6. A control venous abdominal angio CT performed 3 months after transplantation showed normal blood flow at the termino-terminal anastomosis of the hepatic veins of the receptor and the IVC of the new liver (Figure 2).
A written informed consent was obtained from the patient to describe this report.
Discussion
Developmental anomalies of the IVC are relatively rare (5,9,10). They are more common in individuals with congenital heart defects, asplenia or polysplenia syndromes, and biliary atresia. Since the introduction of noninvasive imaging exams, these anomalies have been increasingly described in asymptomatic individuals, as in our patient (5).
Embryogenesis of IVC is a complex process involving the development, regression, anastomosis and replacement of three pairs of embryonic veins: posterior cardinal, subcardinal and supracardinal veins (5). Although most IVC anomalies reported in the literature are single, some patients may have more than one anomaly of different segments of this vein (5,10,11). Our patient presented a complex IVC anomaly: duplication of the infrarenal IVC, agenesia of the hepatic portion of the IVC with azygos continuation of the IVC, and presence of several anomalous veins communicating the common iliac vein and the IVC of one side with the contralateral side.
Duplication of the IVC results of failure of regression of the left supracardinal vein (10,11). The two IVC ascend on each side of the abdominal aorta. While the course of the right-sided IVC is usually normal, the left-sided IVC crosses the aorta to join the right-sided IVC immediately after receiving the respective renal veins (5,10,11). After the coalescing of both IVC, a single IVC continues cranially in a normal course behind the liver to drain into the right atrium.
Agenesis of the hepatic segment of the IVC with azygos continuation is characterized by the presence of IVC from the common iliac vein up to the kidneys (5,12,13). After receiving both renal veins, the IVC passes posterior to the diaphragmatic crura to enter the thorax as a dilated azygos vein. The prominent azygos vein joins the superior vena cava at the normal location in the right paratracheal area. Due to the absence of the hepatic segment of IVC, the hepatic veins drain in a short suprahepatic segment of the IVC (5,12,13). This suprahepatic segment measures only 1-2 cm of length and joins the right atrium immediately after the diaphragm.
Anomalies of the IVC are associated with significant clinical implications. Awareness of these anomalies is necessary to avoid diagnostic pitfalls and surgical complications. A prominent dilation of the azygos vein may mimic a mediastinal mass, such as a paraspinous tumor, lymphadenopathy, or superior vena cava syndrome (6-10). Unnecessary operations or perioperative death following inadvertent ligation of hemiazygos-to-azygos continuation of a left IVC during thoracic surgery has been reported (6,10,14). Duplication of the IVC, mainly in the presence of anomalous veins communicating the common iliac vein and the IVC of both sides, may cause intense bleeding during retroperitoneal surgical procedures (10).
This report is important to alert liver transplant teams of the possibility of an interrupted IVC even in asymptomatic adult individuals. Presence of this anatomical anomaly either in the donor or in the recipient is not a contraindication for liver transplantation (15). Previous diagnosis of the anomaly is important for adequate surgical planning. The presence of a very short suprahepatic portion of the IVC in patients with this anomaly may complicate the anastomosis of this vessel with the suprahepatic IVC of the new liver. A venoplasty of the right, middle, and left hepatic veins allows lengthening of this vessel, facilitating the confection of the anastomosis. Thus, familiarity with these anatomical anomalies is vital to reduce the risk of serious hemorrhage and other operative complications during OLT.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Sato K, Sekiguchi S, Kawagishi N, et al. Hepatic venous reconstruction using the superficial femoral vein in a right-lobe living donor liver transplant patient with interrupted inferior vena cava. Pediatr Transplant 2014;18:E13-7. [PubMed]
- Imamura M, Abraham B, Garcia X, et al. New transplant technique with hemiazygos continuation and interrupted inferior vena cava. Ann Thorac Surg 2013;96:1882-4. [PubMed]
- Itri JN, Heller MT, Tublin ME. Hepatic transplantation: postoperative complications. Abdom Imaging 2013;38:1300-33. [PubMed]
- Levi Sandri GB, Lai Q, Nudo F, et al. Inferior vena cava interruption in a liver transplantation deceased donor. Liver Int 2013;33:647. [PubMed]
- Bass JE, Redwine MD, Kramer LA, et al. Spectrum of congenital anomalies of the inferior vena cava: cross-sectional imaging findings. Radiographics 2000;20:639-52. [PubMed]
- Zinser MJ, Hanto DW. Liver transplantation in a patient with developmental interruption of the inferior vena cava with azygos substitution. Transplant Proc 2012;44:1460-3. [PubMed]
- Hatipoglu S, Olmez A, Ozgor D, et al. Living donor liver transplantation in the absence of inferior vena cava: a case report. Transplant Proc 2012;44:1761-3. [PubMed]
- Matsubara K, Fujimoto Y, Kamei H, et al. Living donor liver transplantation for biliary atresia complicated by situs inversus: technical highlights. Liver Transpl 2005;11:1444-7. [PubMed]
- Yigit H, Yagmurlu B, Yigit N, et al. Low back pain as the initial symptom of inferior vena cava agenesis. AJNR Am J Neuroradiol 2006;27:593-5. [PubMed]
- Chen H, Emura S, Nagasaki S, et al. Double inferior vena cava with interiliac vein: a case report and literature review. Okajimas Folia Anat Jpn 2012;88:147-51. [PubMed]
- Ng WT, Ng SS. Double inferior vena cava: a report of three cases. Singapore Med J 2009;50:e211-3. [PubMed]
- Skeik N, Wickstrom KK, Schumacher CW, et al. Infrahepatic inferior vena cava agenesis with bilateral renal vein thrombosis. Ann Vasc Surg 2013;27:973.e19-23.
- Chaudhary S, Kamyab A, Jacobs M. Congenitally absent inferior vena cava. Am Surg 2013;79:E202-3. [PubMed]
- Orguc S, Tercan M, Bozoklar A, et al. Variations of hepatic veins: helical computerized tomography experience in 100 consecutive living liver donors with emphasis on right lobe. Transplant Proc 2004;36:2727-32. [PubMed]
- Levi Sandri GB, Lai Q, Nudo F, et al. Inferior vena cava interruption in a liver transplantation deceased donor. Liver Int 2013;33:647. [PubMed]


