Novel biomarkers for hepatocellular carcinoma surveillance: has the future arrived?
Hepatocellular carcinoma (HCC) continues to be a major cause of cancer-related mortality and morbidity (1,2). The vast majority of HCC cases occur in those with chronic liver disease, particularly chronic hepatitis B and chronic hepatitis C, which account for up to 85% of HCC cases worldwide (3). Early detection of HCC through surveillance methods has a major impact on patient outcomes, including increased survival (4,5). Efforts to identify HCC in individuals at risk at an early stage are critical to providing highly effective treatment, including primary curative hepatectomy, locoregional ablative therapy, or liver transplantation.
Limitations of current biomarkers
The utilization of serum tumor markers has played a major role in not only surveillance strategies in high-risk populations and achieving a diagnosis of HCC, but also in risk stratification and prediction of recurrence following initial therapy. However, the most widely used tumor marker for HCC, alpha-fetoprotein (AFP), has fallen short in its ability to accurately diagnose HCC, discriminate between high and low risk individuals, and predict high-risk histopathologic features such as microvascular invasion and tumor differentiation. Consequently, AFP has been excluded in some guidelines on HCC surveillance as well as in the diagnostic assessment of hepatic nodules found on surveillance imaging (6).
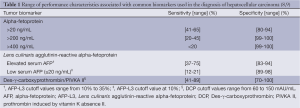
A major limitation associated with serum AFP is its low sensitivity. Large-scale prospective data have revealed that over 45% of patients with HCC may have normal serum AFP levels (7). Multiple case-control and prospective cohort studies have described sensitivities of 41% to 65% and specificities of 80% to 94% for serum AFP levels >20 ng/mL (Table 1) (8). At increasing levels of serum AFP, the sensitivity for detection of HCC declines significantly. Additional limiting factors associated with AFP assessment include variation in serum AFP levels with aminotransferase levels, grade of necroinflammatory activity on liver biopsy, etiology of chronic liver disease, patient ethnicity, and nodule size.
Full table
Several serum markers for HCC have now been identified in addition to AFP; however, data are limited and many have yet to be widely accepted in clinical practice. A fucosylated isoform of AFP reactive to Lens culinaris agglutinin, known as AFP-L3, was initially discovered to be significantly increased in patients with HCC compared with patients with elevated AFP in the absence of HCC (10). Several prospective studies have reported a high sensitivity and specificity associated with AFP-L3 as a diagnostic tool for HCC; however, this marker can only be used in patients with elevated baseline AFP levels. In patients with low AFP levels (≤20 ng/mL), the sensitivity of AFP-L3 can decline significantly (9). Prothrombin induced by vitamin K absence II (PIVKA II), known as des-γ-carboxyprothrombin (DCP), is an abnormal prothrombin molecule also increased in the setting of HCC. Prospective data have reported greater specificity associated with DCP in comparison with AFP, yet the sensitivity of DCP may be diminished. However, the performance characteristics of DCP appear to vary based on the etiology of liver disease, in which its sensitivity may increase in cases with underlying chronic viral hepatitis (11). A large multicenter case-control study evaluating the role of AFP, AFP-L3, and DCP in HCC surveillance found AFP to have the highest sensitivity, although data suggest that a combination of tumor markers may be more effective (11).
Additional serum and plasma biomarkers found to be potential screening tools in the early detection of HCC have included glypican-3 (GPC-3), osteopontin, golgi protein 73 (GP73), microRNA (miRNA), α-1-fucosidase, human telomerase reverse transcriptase, squamous cell carcinoma antigen, and transforming growth factor-β1. GPC-3 is a cell-surface proteoglycan overexpressed in HCC cells and may regulate tumor growth. Although GPC-3 appears to have a high specificity, it has a low sensitivity similar to AFP (12). Likewise, GP73 and miRNAs, such as miR-21, have demonstrated only a slight improvement in performance compared with serum AFP (13). Osteopontin is a glycoprotein expressed in HCC cells, and although it has a higher sensitivity than AFP in the detection of HCC, its specificity remains low and may require a combination with AFP in order to optimize performance (14).
Genome-wide association studies
As the ability to detect genomic variation between individuals has advanced, multiple single nucleotide polymorphisms (SNPs) associated with HCC risk have been identified through various studies involving a wide range of patient populations. Although questions remain regarding the applicability and reproducibility of genomic profiling across different patient groups, some recent reports have identified SNPs that appear to demonstrate a consistent association with risk of HCC (15). However, genomic profiling for assessment of risk of HCC may be limited by a high degree of variation in gene expression based on patient ethnicity and underlying chronic liver disease (16). Further large-scale genomic studies may be required to develop gene expression profiles that can reliably predict risk of HCC. Ultimately an individualized approach based on liver disease etiology and patient ethnicity or a combination of genomic profiling with other biomarkers may be needed to achieve acceptable consistency in identifying individuals at increased risk of HCC incidence or recurrence.
Proteomic and metabolomic analysis
Advancements in analytical techniques involving surface-enhanced laser desorption/ionization time-of-flight mass spectrometry (SELDI-TOF MS), advanced chromatography, and nuclear magnetic resonance spectroscopy have introduced methods of identifying protein and metabolite expression associated with HCC. An array of proteomic studies have now identified multiple serum protein fragments with differential expression in the setting of HCC, many of which could serve as new biomarkers for HCC and may be instrumental in risk assessment, early detection, and surveillance. A limitation of proteomics currently lies in the lack of agreement among various studies in reporting changes in protein expression associated with HCC; however, a meta-analysis of proteomic profiling for HCC noted heat-shock 70-kDa protein (HSP70) and fructose-1,6-bisphosphatase 1 (FPBase) among the most consistently reported proteins with upregulation and downregulation, respectively, in the setting of HCC (17). Likewise, metabolomic studies evaluating changes in lipid and water soluble metabolites found in the blood or urine have paved the way towards identifying a wider array of potential biomarkers for HCC. Methods involving a combination of gene expression and metabolomics, or a combination of different metabolomic platforms, may be required to define markers with highest sensitivity and specificity in the detection of HCC (18-20).
Glycomics and beyond
An area of great interest in biomarker discovery for cancer detection, including HCC, is glycomics. N-glycans are complex polysaccharides bound to biomolecules through N-glycosylation and are found throughout a wide range of biological processes including cell-cell interactions, protein folding, and receptor binding. In particular, specific N-glycosylation patterns may be associated with cancer development (21). Identifying these changes in glycosylation may provide a means to accurately detect HCC tumorigenesis at an early time point.
One recent study published in Hepatology by Kamiyama and colleagues evaluated N-glycosylation alterations in 369 patients with HCC who underwent primary curative hepatectomy compared with 26 controls identified as healthy living related liver transplant donors (22). A novel high-throughput glycoblotting method was utilized for glycomic profiling to identify 67 N-glycans associated with HCC, of which 14 N-glycans had a greater potential to discriminate between individuals with HCC and controls, as defined by receiver operating characteristic analysis. Two serum N-glycans, G3560 and G2890, were identified as significant predictors of overall survival and disease-free survival, respectively, over a median follow up of 5 years (Table 2). Both N-glycans also strongly correlated with other known prognostic markers, including DCP, number and size of tumors, microscopic vascular invasion, and macroscopic vascular invasion.
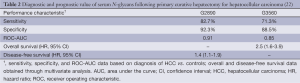
Full table
As demonstrated in this study, glycomic analyses could lead to discovery of alterations in N-glycan profiles that are highly specific to HCC. These data are encouraging and suggest that glycomic biomarkers could play a role in early detection of HCC with a high sensitivity and specificity as well as provide a measure of risk assessment in those with HCC who undergo curative therapy. However, similar to other biomarkers, there may be limitations in glycomic studies associated with variation in study populations. Further investigation will be required to establish reproducibility of these findings and determine its applicability to a wider range of patient groups and liver disease etiologies.
Although challenges remain, a continued effort to identify novel biomarkers utilizing advanced proteomic, metabolomic, and glycomic methodology alongside genomic profiling and existing tumor markers such as AFP will greatly enhance our ability to detect HCC. In light of the complex interplay of cancer pathogenesis, underlying chronic liver disease, and variation among populations at risk of HCC, it is likely that a multimodal approach may be required to develop unique molecular signatures specific to HCC that can identify early patterns corresponding with incidence and recurrence. In addition, this line of research may also reveal further insight into HCC pathogenesis and identify potential therapeutic targets. Although it appears that the future has arrived, we have yet to see how these advances may impact patient outcomes on a larger scale.
Acknowledgements
Disclosure: The author declares no conflict of interest.
References
- Parkin DM, Bray F, Ferlay J, et al. Global cancer statistics, 2002. CA Cancer J Clin 2005;55:74-108. [PubMed]
- Soerjomataram I, Lortet-Tieulent J, Parkin DM, et al. Global burden of cancer in 2008: a systematic analysis of disability-adjusted life-years in 12 world regions. Lancet 2012;380:1840-50. [PubMed]
- Parkin DM. The global health burden of infection-associated cancers in the year 2002. Int J Cancer 2006;118:3030-44. [PubMed]
- Zhang BH, Yang BH, Tang ZY. Randomized controlled trial of screening for hepatocellular carcinoma. J Cancer Res Clin Oncol 2004;130:417-22. [PubMed]
- Sangiovanni A, Del Ninno E, Fasani P, et al. Increased survival of cirrhotic patients with a hepatocellular carcinoma detected during surveillance. Gastroenterology 2004;126:1005-14. [PubMed]
- Bruix J, Sherman M; American Association for the Study of Liver Diseases. Management of hepatocellular carcinoma: an update. Hepatology 2011;53:1020-2. [PubMed]
- Farinati F, Marino D, De Giorgio M, et al. Diagnostic and prognostic role of alpha-fetoprotein in hepatocellular carcinoma: both or neither? Am J Gastroenterol 2006;101:524-32. [PubMed]
- Gonzalez SA, Keeffe EB. Diagnosis of hepatocellular carcinoma: role of tumor markers and liver biopsy. Clin Liver Dis 2011;15:297-306. [PubMed]
- Toyoda H, Kumada T, Tada T. Highly sensitive Lens culinaris agglutinin-reactive α-fetoprotein: a new tool for the management of hepatocellular carcinoma. Oncology 2011;81 Suppl 1:61-5. [PubMed]
- Sato Y, Nakata K, Kato Y, et al. Early recognition of hepatocellular carcinoma based on altered profiles of alpha-fetoprotein. N Engl J Med 1993;328:1802-6. [PubMed]
- Marrero JA, Feng Z, Wang Y, et al. Alpha-fetoprotein, des-gamma carboxyprothrombin, and lectin-bound alpha-fetoprotein in early hepatocellular carcinoma. Gastroenterology 2009;137:110-8. [PubMed]
- Xu C, Yan Z, Zhou L, et al. A comparison of glypican-3 with alpha-fetoprotein as a serum marker for hepatocellular carcinoma: a meta-analysis. J Cancer Res Clin Oncol 2013;139:1417-24. [PubMed]
- Tomimaru Y, Eguchi H, Nagano H, et al. Circulating microRNA-21 as a novel biomarker for hepatocellular carcinoma. J Hepatol 2012;56:167-75. [PubMed]
- Shang S, Plymoth A, Ge S, et al. Identification of osteopontin as a novel marker for early hepatocellular carcinoma. Hepatology 2012;55:483-90. [PubMed]
- Chen K, Shi W, Xin Z, et al. Replication of genome wide association studies on hepatocellular carcinoma susceptibility loci in a Chinese population. PLoS One 2013;8:e77315. [PubMed]
- Villanueva A, Hoshida Y, Battiston C, et al. Combining clinical, pathology, and gene expression data to predict recurrence of hepatocellular carcinoma. Gastroenterology 2011;140:1501-12.e2.
- Liu Z, Ma Y, Yang J, et al. Upregulated and downregulated proteins in hepatocellular carcinoma: a systematic review of proteomic profiling studies. OMICS 2011;15:61-71. [PubMed]
- Budhu A, Roessler S, Zhao X, et al. Integrated metabolite and gene expression profiles identify lipid biomarkers associated with progression of hepatocellular carcinoma and patient outcomes. Gastroenterology 2013;144:1066-75.e1.
- Beyoğlu D, Imbeaud S, Maurhofer O, et al. Tissue metabolomics of hepatocellular carcinoma: tumor energy metabolism and the role of transcriptomic classification. Hepatology 2013;58:229-38. [PubMed]
- Fitian AI, Nelson DR, Liu C, et al. Integrated metabolomic profiling of hepatocellular carcinoma in hepatitis C cirrhosis through GC/MS and UPLC/MS-MS. Liver Int 2014;34:1428-44. [PubMed]
- Ruhaak LR, Miyamoto S, Lebrilla CB. Developments in the identification of glycan biomarkers for the detection of cancer. Mol Cell Proteomics 2013;12:846-55. [PubMed]
- Kamiyama T, Yokoo H, Furukawa J, et al. Identification of novel serum biomarkers of hepatocellular carcinoma using glycomic analysis. Hepatology 2013;57:2314-25. [PubMed]


