Laparoscopic liver resection for hepatocellular carcinoma in patients with cirrhosis
Introduction
Liver resection has been considered one of the most difficult procedures to be performed by laparoscopic means. After the first cholecystectomy (1) performed more than 20 years ago, the development of laparoscopic surgery has been very enthusiastic. Unlike many medium-sized operations such as laparoscopic hernia repair, splenectomy and adrenalectomy the development of laparoscopic hepatectomy has been slow (2-4). The initial indication of laparoscopic liver resection was mainly limited to benign conditions (5). With increasing number of successful reports, nowadays the indications was been broadened to other malignant condition liver colorectal liver metastasis and hepatocellular carcinoma (HCC) (6-9).
The gold standard
Open hepatectomy has been a well-established treatment option for HCC even in patients with liver cirrhosis. In our center, we performed more than 250 cases of the liver resection per year. Amongst those, 75% of the cases were hepatitis B carrier where liver cirrhosis is a common finding during the operation. In recent 10 years, we observed a constant good results of hepatectomy for HCC despite an older patient population, a higher incidence of comorbid illness, a higher incidence of cirrhosis, and worse liver function in patients (10). The operation mortality rate nowadays for major hepatectomy in patients with cirrhosis was 4.3% and operation mortality rate for minor hepatectomy in patients with cirrhosis was 1.5% (11). It is not difficult to imagine the slow development pace of laparoscopic liver resection in the presence of well high quality performance of the open approach.
Difficulties of liver resection in patients with liver cirrhosis
Liver resection remains one of the most challenging procedures in surgery. The liver is anatomically divided into different sections according to its complex vasculatures. Bleeding, biliary fistula, post-operative liver failure and mortality could happened even after a simple minor hepatectomy (12). In Asia, the incidence of HCC is highest in the world due to the presence of concomitant hepatitis B infection. Hepatitis B related HCC usually associated with liver cirrhosis in Asian countries. Without a proper screening program, most of the patients with HCC are considered unresectable due to the late presentation of the symptom (13). Only 25% of the patients can received live resection at the moment the diagnosis is made. The presence of portal hypertension, splenomegaly, presence of gastric or esophageal varices and thrombocytopenia make hepatectomy more difficult when compared to liver resection in the western countries (14). The major hurdle to laparoscopic liver hepatectomy is obvious. It seems very difficult if not impossible to perform such a difficult operation in difficult patients with minimally access surgery.
Technical issues
We believed that safe hepatectomy can be performed in patients with HCC even in the presence of cirrhosis. The selection criteria of laparoscopic liver resection follow exactly the same principle of open surgery. There should be absence of extrahepatic disease, absence of tumor thrombus in the main portal vein and inferior vena cava and anatomically feasible for liver resection. Liver function assessment was based largely on the result of the indocyanine green (ICG) clearance test. An ICG retention rate of 14% at 15 min after injection was considered favorable for major hepatectomy. For minor hepatectomy, the cut-off value for ICG clearance was 22% (11). In laparoscopic approach, the technique should be comparable to that of open approach. For patients receiving major liver resection, the portal pedicle will be dissected clearly from the Glisson capsule and the portal vein, hepatic artery and bile duct were separately controlled and divided. The patient was usually placed in the Lloyd-Davis position. The primary surgeon stood between the legs with one assistant on each side. Pneumoperitoneum was usually done by subumbilical incision. Three to four working ports sized between 5 and 12 mm were used. This allow the use of an ultrasonic dissector like Harmonic scalpel or Thunder beat and a CUSA for parenchymal transection (15,16). Nowadays, the new energy devices can produce good sealing effects to vessels up to 7 mm in diameters. These could assist effective liver parenchymal transection in anatomic liver resection where major bile ducts were located away from the transection plane.
Intraoperative ultrasound was performed as with the patients receiving the open approach. The small vessels were controlled with multi-fired metal clips. The major hepatic veins were controlled with vascular staplers. Hemostasis was performed using metal clips, diathermy, and suturing. The liver was delivered through an incision not larger than the largest diameter of the delivered specimen. Usually in a pfannenstiel incision were the wound would become less visible after the operation. Usually no drainage tube was placed (16).
One of the major breakthroughs in laparoscopic liver resection is the rapid development of the high definition unit of the laparoscopic camera processor. Crystal clear image with magnification make meticulous dissection of the vital structure of the liver possible. Apart from clear visualization, the application of the positive pneumoperitoneum pressure makes liver parenchymal transection less difficult (17-19).
In open approach, in order to prevent venous oozing from liver parenchymal transection, careful administration of intravenous fluid and meticulous central venous pressure control was administrated. With the help of vasodilators and diuretics, the anesthesiologist will cautiously keep the CVP at preferably less than 5 cm water. In laparoscopic approach, the venous oozing can be effectively manipulated by elevation of the pneumoperitoneum pressure (11). This is particularly important for patients with cirrhosis where venous oozing secondary to portal hypertension is a common phenomenon. It has been shown that laparoscopic hepatectomy performed in a range between 10-14 mmHg is safe (20-23). There has not been a single report of major gas embolism event that has led to a major complication (Calvien-Dindo > II) due to pneumoperitoneum (24,25).
Indications and advantages
We started with our initial laparoscopic liver resection for cancers with small peripheral lesions in patients with liver metastasis. Our initial result demonstrated that laparoscopic liver resection in selected patients can produce some favorable outcome. Comparing the laparoscopic group with the open resection group, the median operating time was 180 vs. 210 min (P=0.059), the median blood loss was 200 vs. 310 mL. Hospital stay was 4.5 vs. 7 days (9). The extent of resection has become wider when experience accumulated. Liver resection for HCC in cirrhotic patients is possible. In fact, laparoscopic minor resection for patients with cirrhosis may be advantageous. A large wound could be avoided particularly when the lesion is located in the posterior section of the right side of the liver. Bleeding complication, infection of the wound, hernia formation of the wound is more common if the incision is bigger particularly in patients with cirrhosis and portal hypertension. In comparison to laparoscopic liver resection, patients with liver cirrhosis prone to developed ascites after open hepatectomy with a larger wound (26). Probably it is because laparoscopic liver resection causes fewer disturbances to the collateral vessels in the abdominal wall. It has been observed that laparoscopic liver resection will provide a less blood loss, shorter operation time and shorter hospital stay. We have reported our initial result in Annals of Surgery. With the laparoscopic group compared with the open resection group, operation time was 232.5 vs. 204.5 min, blood loss was 150 vs. 300 mL, hospital stay was 4 vs. 7 days, postoperative complication was 2 (6.3%) vs. 12 (18.8%) (16).
Currently laparoscopic left lateral sectionectomy has been considered a standard practice in many of the centers where there is expertise in hepatobiliary and laparoscopic surgery (27,28).
Laparoscopic major hepatectomy has been more controversial particularly when it involved patients with HCC and cirrhosis. The same argument applied to lesion located in more difficult location of the liver like sections 1,7,8 and superior part of section (29). This would be question of patients’ safety vs. the advantage of patients’ gain through a smaller wound. Unlike minor liver resection, at least at this moment, there is not enough evidence to show that laparoscopic liver resection is a more favorable surgical option in patients with liver cirrhosis. The median operation time was longer and the median blood loss was not less if not more (30). Although laparoscopic major liver resection is technically feasible in patients with moderate size tumor, the reported number of cases performed is still small. Since not every cases with HCC is favorable for laparoscopic resection, the experience accumulated for laparoscopic liver resection is still in its early phase and many of the reported cases series probably has not pass its learning curve phase as reflected by the number of cases performed (31).
For cancer treatment, long term survival outcome is more important than the approach of the operative technique applied. Since the principle of laparoscopic hepatectomy is to mimic the open approach without compromise, similar oncological outcome has been observed. In our center, comparing the laparoscopic group with the open resection group for colorectal liver metastasis, the median survival was 69.4 vs. 42.1 months, and the disease-free survival was 9.8 vs. 10.9 months (9). For patients with HCC, with the laparoscopic hepatectomy compared with the open resection, disease-free survival was 78.5 vs. 29 months, and overall survival was 92 vs. 71 months. The disease-free survival for stage II HCC was 22.1 vs. 12.4 months (16).
There are several systemic reviews and meta-analysis articles published to investigate the role of laparoscopic liver hepatectomy (30,32-36). It is generally observed that favorable outcome is observed in terms of operative blood loss, blood transfusion requirement, and length of stay in the laparoscopic hepatectomy groups. There was no difference in terms of surgical margin, overall and disease free survival when laparoscopic approach was compared to conventional open approach. There was only one meta-analysis investigating the results of laparoscopic liver resection for HCC patients with cirrhosis involving 4 nonrandomized studies (34). The results showed that laparoscopic approach has a better short term outcomes with less blood loss, wider resection margin and shorter hospital stays. However, this information has to be interpreted with caution. All of the studies involved in all these systemic review or meta-analysis are non-randomized trial. Most of the studies involved included mainly minor liver resection or technically straight forward operations. The effect of publication bias is needed to be addressed. Centers with unfavorable outcome by laparoscopic approach may not report these results. Randomized controlled trials in processes will definitely provide better reflection of actual situation.
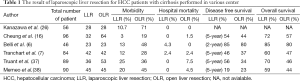
Table 1 summarized the result of laparoscopic liver resection for HCC patients with cirrhosis performed in various center (6,7,16,26,37,38). The experience reported on laparoscopic liver resection on cirrhotic liver is still limited but undoubtedly there is an overwhelming enthusiasm on this topic. The number of published articles has been increasing throughout the year.
Full table
Conclusions
Laparoscopic liver resection in cirrhotic liver remained a technically challenging procedure. It has to be performed in centers with expertise in (I) surgeons who can performed complicated liver surgery; (II) surgeons who are experienced in laparoscopic technique; and (III) high volume center of liver surgery. Careful case selection without compromise to patients’ safety is the key to success and favorable surgical outcome.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Mühe E. Laparoscopic cholecystectomy. Z Gastroenterol Verh 1991;26:204-6. [PubMed]
- Barczyński M, Konturek A, Nowak W. Randomized clinical trial of posterior retroperitoneoscopic adrenalectomy versus lateral transperitoneal laparoscopic adrenalectomy with a 5-year follow-up. Ann Surg 2014;260:740-7. [PubMed]
- Mason RJ, Moazzez A, Sohn HJ, et al. Laparoscopic versus open anterior abdominal wall hernia repair: 30-day morbidity and mortality using the ACS-NSQIP database. Ann Surg 2011;254:641-52. [PubMed]
- Musallam KM, Khalife M, Sfeir PM, et al. Postoperative outcomes after laparoscopic splenectomy compared with open splenectomy. Ann Surg 2013;257:1116-23. [PubMed]
- Shimada M, Hashizume M, Maehara S, et al. Laparoscopic hepatectomy for hepatocellular carcinoma. Surg Endosc 2001;15:541-4. [PubMed]
- Belli G, Fantini C, D’Agostino A, et al. Laparoscopic versus open liver resection for hepatocellular carcinoma in patients with histologically proven cirrhosis: short- and middle-term results. Surg Endosc 2007;21:2004-11. [PubMed]
- Tranchart H, Di Giuro G, Lainas P, et al. Laparoscopic resection for hepatocellular carcinoma: a matched-pair comparative study. Surg Endosc 2010;24:1170-6. [PubMed]
- Cheung TT, Ng KK, Poon RT, et al. A case of laparoscopic hepatectomy for recurrent hepatocellular carcinoma. World J Gastroenterol 2010;16:526-30. [PubMed]
- Cheung TT, Poon RT, Yuen WK, et al. Outcome of laparoscopic versus open hepatectomy for colorectal liver metastases. ANZ J Surg 2013;83:847-52. [PubMed]
- Fan ST, Lo CM, Liu CL, et al. Hepatectomy for hepatocellular carcinoma: toward zero hospital deaths. Ann Surg 1999;229:322-30. [PubMed]
- Fan ST, Mau Lo C, Poon RT, et al. Continuous improvement of survival outcomes of resection of hepatocellular carcinoma: a 20-year experience. Ann Surg 2011;253:745-58. [PubMed]
- Ishizawa T, Mise Y, Aoki T, et al. Surgical technique: new advances for expanding indications and increasing safety in liver resection for HCC: the Eastern perspective. J Hepatobiliary Pancreat Sci 2010;17:389-93. [PubMed]
- Yau T, Tang VY, Yao TJ, et al. Development of Hong Kong Liver Cancer staging system with treatment stratification for patients with hepatocellular carcinoma. Gastroenterology 2014;146:1691-700. [PubMed]
- Imamura H, Sano K, Sugawara Y, et al. Assessment of hepatic reserve for indication of hepatic resection: decision tree incorporating indocyanine green test. J Hepatobiliary Pancreat Surg 2005;12:16-22. [PubMed]
- Cheung TT, Poon RT. Synchronous resections of primary colorectal tumor and liver metastasis by laparoscopic approach. World J Hepatol 2013;5:298-301. [PubMed]
- Cheung TT, Poon RT, Yuen WK, et al. Long-term survival analysis of pure laparoscopic versus open hepatectomy for hepatocellular carcinoma in patients with cirrhosis: a single-center experience. Ann Surg 2013;257:506-11. [PubMed]
- Farges O, Goutte N, Dokmak S, et al. How surgical technology translates into practice: the model of laparoscopic liver resections performed in France. Ann Surg 2014;260:916-21. [PubMed]
- Fuks D, Cauchy F, Ftériche S, et al. Laparoscopy Decreases Pulmonary Complications in Patients Undergoing Major Liver Resection: A Propensity Score Analysis. Ann Surg 2015. [Epub ahead of print]. [PubMed]
- Cheung TT, Poon RT, Lo CM. Reply to Letter: "Long-term Survival Analysis of Pure Laparoscopic Versus Open Hepatectomy for Hepatocellular Carcinoma in Patients With Cirrhosis: A Single-center Experience Ann Surg 2015;262:e20-1. [PubMed]
- Honda G, Kurata M, Okuda Y, et al. Totally laparoscopic hepatectomy exposing the major vessels. J Hepatobiliary Pancreat Sci 2013;20:435-40. [PubMed]
- Troisi RI, Van Huysse J, Berrevoet F, et al. Evolution of laparoscopic left lateral sectionectomy without the Pringle maneuver: through resection of benign and malignant tumors to living liver donation. Surg Endosc 2011;25:79-87. [PubMed]
- Aldrighetti L, Pulitanò C, Arru M, et al. Ultrasonic-mediated laparoscopic liver transection. Am J Surg 2008;195:270-2. [PubMed]
- Gayet B, Cavaliere D, Vibert E, et al. Totally laparoscopic right hepatectomy. Am J Surg 2007;194:685-9. [PubMed]
- Jayaraman S, Khakhar A, Yang H, et al. The association between central venous pressure, pneumoperitoneum, and venous carbon dioxide embolism in laparoscopic hepatectomy. Surg Endosc 2009;23:2369-73. [PubMed]
- Schmandra TC, Mierdl S, Hollander D, et al. Risk of gas embolism in hand-assisted versus total laparoscopic hepatic resection. Surg Technol Int 2004;12:137-43. [PubMed]
- Kanazawa A, Tsukamoto T, Shimizu S, et al. Impact of laparoscopic liver resection for hepatocellular carcinoma with F4-liver cirrhosis. Surg Endosc 2013;27:2592-7. [PubMed]
- Dokmak S, Raut V, Aussilhou B, et al. Laparoscopic left lateral resection is the gold standard for benign liver lesions: a case-control study. HPB (Oxford) 2014;16:183-7. [PubMed]
- Hasegawa Y, Nitta H, Sasaki A, et al. Laparoscopic left lateral sectionectomy as a training procedure for surgeons learning laparoscopic hepatectomy. J Hepatobiliary Pancreat Sci 2013;20:525-30. [PubMed]
- Han HS, Yoon YS, Cho JY, et al. Laparoscopic liver resection for hepatocellular carcinoma: korean experiences. Liver Cancer 2013;2:25-30. [PubMed]
- Nguyen KT, Marsh JW, Tsung A, et al. Comparative benefits of laparoscopic vs open hepatic resection: a critical appraisal. Arch Surg 2011;146:348-56. [PubMed]
- Hibi T, Cherqui D, Geller DA, et al. International Survey on Technical Aspects of Laparoscopic Liver Resection: a web-based study on the global diffusion of laparoscopic liver surgery prior to the 2nd International Consensus Conference on Laparoscopic Liver Resection in Iwate, Japan. J Hepatobiliary Pancreat Sci 2014;21:737-44. [PubMed]
- Yin Z, Fan X, Ye H, et al. Short- and long-term outcomes after laparoscopic and open hepatectomy for hepatocellular carcinoma: a global systematic review and meta-analysis. Ann Surg Oncol 2013;20:1203-15. [PubMed]
- Xiong JJ, Altaf K, Javed MA, et al. Meta-analysis of laparoscopic vs open liver resection for hepatocellular carcinoma. World J Gastroenterol 2012;18:6657-68. [PubMed]
- Twaij A, Pucher PH, Sodergren MH, et al. Laparoscopic vs open approach to resection of hepatocellular carcinoma in patients with known cirrhosis: systematic review and meta-analysis. World J Gastroenterol 2014;20:8274-81. [PubMed]
- Fancellu A, Rosman AS, Sanna V, et al. Meta-analysis of trials comparing minimally-invasive and open liver resections for hepatocellular carcinoma. J Surg Res 2011;171:e33-45. [PubMed]
- Zhou YM, Shao WY, Zhao YF, et al. Meta-analysis of laparoscopic versus open resection for hepatocellular carcinoma. Dig Dis Sci 2011;56:1937-43. [PubMed]
- Truant S, Bouras AF, Hebbar M, et al. Laparoscopic resection vs. open liver resection for peripheral hepatocellular carcinoma in patients with chronic liver disease: a case-matched study. Surg Endosc 2011;25:3668-77. [PubMed]
- Memeo R, de’Angelis N, Compagnon P, et al. Laparoscopic vs. open liver resection for hepatocellular carcinoma of cirrhotic liver: a case-control study. World J Surg 2014;38:2919-26. [PubMed]


