Surgery for gallstone disease during pregnancy does not increase fetal or maternal mortality: a meta-analysis
Introduction
Gallstone-related disease (GRD) encompasses a wide spectrum of clinical entities ranging from biliary colic to acute gallstone pancreatitis. GRD is one of the most common general surgical emergencies during pregnancy (1-3) and complicates between 0.05-0.8% of pregnancies (4-6). The management of GRD during pregnancy remains a significant challenge to the general surgeon and obstetrician. GRD during pregnancy has been traditionally managed conservatively with surgery being reserved for patients in whom symptoms are persistent. This traditional dogma has been challenged by two observations. Firstly, fetal death rate is higher following conservative treatment than after laparoscopic cholecystectomy (7). Secondly conservative management of GRD has reported patient readmission rates and symptom recurrence rates of between 40-92% (7-9).
There is no consensus as to the optimal management of the pregnant patient with GRD although a review by Date et al. has tentatively suggested recommendations (10). In this review the authors suggested that although the results of conservative and surgical management of GRD are similar in terms of maternal and fetal morbidity and mortality, laparoscopic cholecystectomy might be the preferred option because of the increased risks of symptom relapse and hospital readmission with conservative management as suggested above (8,10,11). Emerging evidence suggests that laparoscopic cholecystectomy appears to be a safe procedure during all trimesters of pregnancy (12) but probably best carried out during the second trimester as fetal organogenesis is complete (10,13). The latter is with the proviso that open conversion may be required. In this study we reviewed the literature to assess whether laparoscopic/open cholecystectomy for GRD during pregnancy increases the risk of fetal and maternal mortality and the frequency of preterm delivery.
Materials and methods
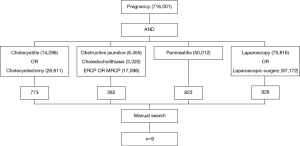
A computerised search was made of the PubMed and MEDLINE databases for the period from January 1966 through December 2013. The MESH headings “cholecystitis”, “cholecystectomy”, “obstructive jaundice”, “choledocholithiasis”, “laparoscopy”, “laparoscopic surgery”, “biliary colic”, “acute cholecystitis”, “endoscopic retrograde cholangiopancreatography”, and “pancreatitis” were searched. These searches were combined using the term “OR”. Then Medline Subject Heading “pregnancy” was searched. The two searches were then combined using the term “and”. Abstracts of the articles found were scrutinised to identify the original human studies and also to exclude editorials, review articles, and letters to editors. The full text of each of the human studies was obtained and studied. Manual cross-referencing was then carried out, based on the bibliography of articles identified in the original searches, to ensure inclusion of all possible studies. Articles were excluded if they were duplicate studies on the same patient group. Figure 1 demonstrates how the included studies were derived for the study.
Statistical analyses
The results of the included studies were pooled using meta-analysis techniques. Fixed effect Mantel-Haenszel models were used where heterogeneity was found to be non-significant. The analyses were performed using Review Manager 5 [REF: Review Manager (RevMan) (Computer program). Version 5.0. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2008.], with P<0.05 deemed to be indicative of statistical significance
Results
Nine studies were identified for inclusion that compared conservative versus operative management for GRD in pregnancy, with a total sample size of 470, all of whom were initially treated conservatively. No maternal mortality was reported in any of the studies. In our study we have focused upon the incidence of premature delivery and fetal mortality.
Figure 2 reports the results of the meta-analysis of premature delivery rates. In total, premature delivery occurred in 5/132 (3.8%) of the patients in the surgical group and 23/338 (6.8%) of those treated conservatively. Heterogeneity was non-significant (I2=36%, P=0.17), hence a fixed effects model was used. The resulting pooled odds ratio for surgically, relative to conservatively treated patients was 0.67 (95% CI: 0.29-1.56). This was non-significant (P=0.36), hence there is no evidence of a significant difference between the rates of premature delivery between the two patient groups.
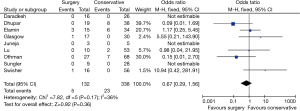
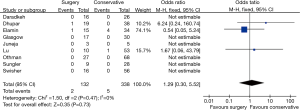
Figure 3 reports the results of the meta-analysis of fetal mortality rates. In total, fetal mortality occurred in 2/132 (1.5%) of the patients in the surgical group and 5/338 (1.5%) of those treated conservatively. Heterogeneity was non-significant (I2=0%, P=0.47), hence a fixed effects model was used. The resulting pooled odds ratio for surgically, relative to conservatively treated patients was 1.29 (95% CI: 0.30-5.52). This was non-significant (P=0.73), hence there is no evidence of a significant difference between the rates of fetal mortality between the two patient groups. Only one study had a high rate of preterm delivery and fetal loss (14). Apart from this report, there were two preterm deliveries each in the surgical and conservative groups.
Discussion
There remains an ongoing debate as to whether patients with GRD should undergo cholecystectomy during pregnancy. Generally laparoscopic cholecystectomy is considered safe during the second trimester of pregnancy because it is associated with fewer spontaneous abortions than in the first trimester (6). Although more recent studies suggest that laparoscopic cholecystectomy can be performed safely in all three trimesters of pregnancy with no maternal or fetal mortality (15,16). Our review did not show a statistically significant effect in fetal mortality and preterm delivery between the conservative and surgery groups. Although not assessed in our review, previous studies suggest that surgical intervention for GRD has increased risks in non-Caucasian ethnicity, older aged patients, obesity, patients with previous abdominal surgery and diabetics (5). Hence patients with GRD and these co-morbidities should be managed with intravenous fluids, intravenous antibiotics and inconjunction with an obstetrician. In the absence of these risk factors surgical interventional should be considered if the symptoms of biliary colic persist or worsen despite dietary changes, results in multiple hospital admissions or weight loss, intolerance to adequate oral intake, increasing abdominal tenderness and/or patient preference (17). In addition it must be remembered that surgical intervention will reduce hospital readmissions and lead to symptom resolution. Furthermore pregnant patients with GRD should be managed in a centre with neonatology expertise including access to neonatal resuscitation and neonatal intensive care (11).
In Dhupar et al. study 19 patients underwent laparoscopic cholecystectomy during pregnancy compared to 39 patients who were managed conservatively for GRD. There was a significant risk of short- and long-term morbidity in the conservative group (17). Cholecystectomy was shown to be safe during all trimesters with no conversion to open surgery required and a low rate of post-operative complications. There was no reported maternal or fetal mortality. This study is further supported by our review. However, our study has not considered the role of conservative, surgical and indeed endoscopic management of complex GRD such as choledocholithiasis (18,19). This suggests that fetal loss maybe disease specific and independent of surgery. In addition, this area of surgical practice is likely influenced by publication bias and this must be bore in mind when analyzing the present review. In addition there are other limitations with the present review including the retrospective nature of some of the included studies and the lack of long-term follow-up of neonates following either surgical versus conservative management.
Cholecystectomy, preferably laparoscopic, for GRD during pregnancy is probably the optimal management of this condition based on available data in term of fetal mortality and preterm delivery (20). However GRD is a manifestation of many different clinical conditions including biliary colic, acute cholecystitis, chronic cholecystitis and pancreatitis. Unfortunately of the 9 studies included in the present meta-analysis, 4 studies did not differentiate between the above conditions or instead studied only one of these conditions. Hence in this review we were unable to perform a sub-group analysis with reference to the different forms of GRD.
The only limiting factor governing operative intervention in GRD during pregnancy should be the surgeon’s operative experience (10).
Conclusions
In summary on the basis of the available evidence cholecystectomy can be considered safe in pregnancy in terms of pre-term delivery and fetal loss.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by institutional ethics board.
References
- Ghumman E, Barry M, Grace PA. Management of gallstones in pregnancy. Br J Surg 1997;84:1646-50. [PubMed]
- Kammerer WS. Nonobstetric surgery during pregnancy. Med Clin North Am 1979;63:1157-64. [PubMed]
- Daradkeh S, Sumrein I, Daoud F, et al. Management of gallbladder stones during pregnancy: conservative treatment or laparoscopic cholecystectomy? Hepatogastroenterology 1999;46:3074-6. [PubMed]
- Gurbuz AT, Peetz ME. The acute abdomen in the pregnant patient. Is there a role for laparoscopy? Surg Endosc 1997;11:98-102. [PubMed]
- Ko CW. Risk factors for gallstone-related hospitalization during pregnancy and the postpartum. Am J Gastroenterol 2006;101:2263-8. [PubMed]
- McKellar DP, Anderson CT, Boynton CJ, et al. Cholecystectomy during pregnancy without fetal loss. Surg Gynecol Obstet 1992;174:465-8. [PubMed]
- Jelin EB, Smink DS, Vernon AH, et al. Management of biliary tract disease during pregnancy: a decision analysis. Surg Endosc 2008;22:54-60. [PubMed]
- Swisher SG, Schmit PJ, Hunt KK, et al. Biliary disease during pregnancy. Am J Surg 1994;168:576-9; discussion 580-1. [PubMed]
- Othman MO, Stone E, Hashimi M, et al. Conservative management of cholelithiasis and its complications in pregnancy is associated with recurrent symptoms and more emergency department visits. Gastrointest Endosc 2012;76:564-9. [PubMed]
- Date RS, Kaushal M, Ramesh A. A review of the management of gallstone disease and its complications in pregnancy. Am J Surg 2008;196:599-608. [PubMed]
- Lu EJ, Curet MJ, El-Sayed YY, et al. Medical versus surgical management of biliary tract disease in pregnancy. Am J Surg 2004;188:755-9. [PubMed]
- Machado NO, Machado LS. Laparoscopic cholecystectomy in the third trimester of pregnancy: report of 3 cases. Surg Laparosc Endosc Percutan Tech 2009;19:439-41. [PubMed]
- Bani Hani MN, Bani-Hani KE, Rashdan A, et al. Safety of endoscopic retrograde cholangiopancreatography during pregnancy. ANZ J Surg 2009;79:23-6. [PubMed]
- Elamin Ali M, Yahia Al-Shehri M, Abu-Eshy S, et al. Is surgical intervention in acute cholecystitis in pregnancy justified? J Obstet Gynaecol 1997;17:435-8. [PubMed]
- Buser KB. Laparoscopic surgery in the pregnant patient: results and recommendations. JSLS 2009;13:32-5. [PubMed]
- Juneja SK, Gupta S, Virk SS, et al. Acute pancreatitis in pregnancy: A treatment paradigm based on our hospital experience. Int J Appl Basic Med Res 2013;3:122-5. [PubMed]
- Dhupar R, Smaldone GM, Hamad GG. Is there a benefit to delaying cholecystectomy for symptomatic gallbladder disease during pregnancy? Surg Endosc 2010;24:108-12. [PubMed]
- Kim YW, Zagorski SM, Chung MH. Laparoscopic common bile duct exploration in pregnancy with acute gallstone pancreatitis. JSLS 2006;10:78-82. [PubMed]
- Sungler P, Heinerman PM, Steiner H, et al. Laparoscopic cholecystectomy and interventional endoscopy for gallstone complications during pregnancy. Surg Endosc 2000;14:267-71. [PubMed]
- Glasgow RE, Visser BC, Harris HW, et al. Changing management of gallstone disease during pregnancy. Surg Endosc 1998;12:241-6. [PubMed]