In vitro three dimensional culture of hepatocellular carcinoma to measure prognosis and responsiveness to chemotherapeutic agents
Introduction
Understanding the prognosis for patients with hepatocellular carcinoma (HCC) helps determine the most appropriate treatment. This is best understood when considering liver transplantation in patients whose HCC is confined to the liver. Despite complete resection of the cancer and the tumor bearing liver, recurrence of HCC occurs. The number and size of tumors is used to predict outcomes after liver transplantation. The Milan and University of California at San Francisco (UCSF) criteria are presently the most widely used systems to allocate grafts for transplantation: the former includes patients with a solitary tumor ≤5 cm or ≤3 tumors (each ≤3 cm), while the latter includes patients with a solitary tumor ≤6.5 cm or ≤3 tumors (each ≤4.5 cm) and a total tumor diameter ≤8 cm (1,2). We analysed our own experience and found HCC recurrence rates of 6%, 67% and 50% for patients with tumors within Milan criteria, within UCSF but not Milan and select patients outside of UCSF criteria, respectively (3).
Tumor morphology has also been used to predict outcome. Parfitt and colleagues categorized tumors using four pathological features into high, intermediate and low grades with HCC recurrence rates of <5%, 40–65%, and >95% respectively (3).
Genetic features of HCC may be responsible for its ability to grow and metastasize. Several methods are now available to develop a profile of a tumor from its genome, and expressed RNA and proteins. When combined, sometimes called multi-omics, these methods produce an enormous amount of data from which it is difficult to extract prognostic signals (4). Miao and colleagues used differential multi-omics to identify TTK, a kinase with links to p53 and a mitotic check point regulator, as a potential prognostic indicator (5). High TTK expressors were three times more likely to develop recurrent HCC after resection compared to low expressors. Several other genes have been identified as possible prognostic markers in HCC including beta-catenin (6), annexinA1 (7), CHD1L (8), MAGE-D2 (9), and ctBP2 (10).
The ability of a tumor to grow and to metastasize determines its resectability and its likelihood to recur. Building a phenotype from these characteristics should be a powerful biomarker of prognosis because it combines all the features previously discussed. Standard in vitro culture has proven to be a poor tool because of the poor mimicry of the natural tumor environment (11,12). Three-dimensional tissue culture (3DTC) has advantages over traditional culture methods that allow cells to grow in a manner similar to how they grow in vivo. The 3D matrix allows the cells to naturally stack rather than grow as flat mono-layers where they have a very high surface area interacting with non-biological material (13). In these 3D cultures, cancer cells are shown to grow and express genes as they do in situ but not in flat culture systems (13). The beneficial properties of 3D culture that allow cancerous tissues to grow more naturally make it the preferred choice for cancer drug screening of excised tissue (14).
Here we describe a system that utilizes 3D culture of excised tumours to research the tumor grade and chemosensitivity and attempt to correlate it to patient survival and histology score.
Methods
Patients
Approval for use of surgical specimens and collection of retrospective patient information was granted by the office of research ethics at the University of Western Ontario (REB number #11353E) and is in accordance with the declaration of Helsinki. Informed consent was gathered from each patient prior to surgery. Each patient willingly donated surgical specimens to this study.
3D tissue culture
The assay system has been reported previously (15,16). Briefly, tumor samples were placed in a cold sterile saline solution for transport. The tissue samples were subsequently transferred to a sterile petri dish and immersed in cold DMEM (Gibco BRL, Burlington, Canada). The tissue was then sliced into 1 mm3 pieces with a scalpel and implanted into a 48 well multi-well plate (Corning, NY, USA) containing a collagen gel matrix. The collagen type I gel (Vitrogen 100) obtained from Advanced Biomatrix Inc. (Palo Alto, CA, USA) was used at a concentration of 1 mg/mL. Once the surface of the gel is patent, an overlay of DMEM with 20% FBS was added. Six (n=6) samples are chosen at random for each treatment. The following concentrations of agents were added individually to DMEM in wells designed to test tumor responsiveness to the agent: 5 fluorouracil (5FU) 10 µg/mL; doxorubicin 4 µg/mL; docetaxel 3 µg/mL; irinotecan 5 µg/mL; or taxol 10 µg/mL. In these wells the agent diffused toward the tumor tissue. The plates were then incubated at 37 °C and monitored microscopically to measure the distance that satellite tumors migrated from the central block into the surrounding matrix for up to 10 days. To account for slight variability between sample replicates, the migration distance is measured from the fragment edge out into the matrix at six independent points.
Histology
Operative tissue was sectioned and stained with H&E before being evaluated by a pathologist who was unaware of the 3DTC results. Tissues were graded as low, intermediate, or high on the scale described previously (3). Patients were followed indefinitely. Patients who were no longer attending the hospital were contacted in August 2015 for review. Patient outcomes were categorized as: (I) alive, no recurrence; (II) alive with recurrent HCC; (III) dead. For those who died we tried to determine if death was due to recurrent HCC.
Data analysis and statistics
The invasion of tumor cells across viable wells was averaged and quantified each day measured. The mean invasive distance (µm) for each day was compared across HCC grades using ANOVA.
Mean invasive distance of samples treated with chemotherapeutic agents was expressed relative to control samples. The primary outcome measure for assessment of prognostic and predictive markers was survival, calculated from the date of first surgery to the date of death or date last known to be alive in days. Patients who had recent clinical contact were considered alive and were censored. Kaplan Meier survival curves were computed using log rank test statistic. A Cox regression survival model was used to investigate relationship of clinical parameters (age, grade, extent of resection) on survival.
Results
Seventeen patients were recruited of whom four did not fit our criteria for the following reasons: metastatic colorectal cancer (n=1), metastatic gastrointestinal stromal tumour (n=1), metastatic leiomyosarcoma (n=1) and one patient with HCC had a concurrent pancreatic adenocarcinoma. Of the 13 included patients, six had hepatitis C virus, three had hepatitis B virus and four had other causes of cirrhosis (alcohol and non-alcoholic steatohepatitis). The tumor grades were low (n=3; 23%); intermediate (n=8; 62%) and high (n=2; 15%). Three patients (21%) were treated with chemoembolization of the liver prior to surgery. After transplantation, 6 patients (43%) were given chemotherapy (n=1 radiation with xeloda, n=4 xeloda alone, n=1 sorafenib). All patients have been followed for over 5 years: six (46%) patients are alive with no recurrence, one (8%) patient is alive with recurrence of HCC, and six (46%) patients are deceased. Of the deceased patients, three deaths were attributed to HCC. The median time of survival of the deceased patients was 12 months post transplant (range, 11–21 months).
We assessed 13 specimens collected from patients with HCC by 3DTC. Three tumour samples did not grow but these tumors appeared to be viable histologically, with one being graded low and two graded as intermediate. Of these three patients, one had been treated with chemoembolization but histology demonstrated viable tumor of intermediate grade. Of the 13 confirmed HCC samples, 10 grew in 3D culture for up to 10 days (median, 5 d; range, 1–10 d). The average first and last measured migration distances (µm) were 108.3±103.7 and 332.7±351.7 respectively. Migration distances (µm) were 188.8±104.3, 104.5±111.7 and 39.6±32.4 for tumors categorized as high, intermediate and low grade, respectively. Two of the three patients who had received chemoembolization demonstrated tumor growth and migration on 3DTC: 180.0±68.1 and 325 µm. Migration distance was 145±296.9 µm for survivors compared to 80±258.8 µm in samples from non-survivors.
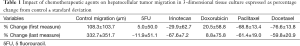
The tumor samples were also cultured in the presence of five chemotherapeutic agents separately (Table 1). Tumor migration was inhibited by irinotecan, paclitaxel and docetaxel (−68%±7%, −61%±19% and −60%±21%, respectively) whereas the effect was variable with 5FU and doxorubicin (−12%±51% and 9%±76% respectively).
Full table
Discussion
HCC is considered a very lethal cancer. When identified early, the best prognosis follows partial lobectomy or complete liver resection with transplantation (1). For advanced unresectable HCC, sorafenib is the recommended systemic treatment (17), although small clinical trials have shown benefit from systemic treatment with capecitabine (18), doxorubicin (19), gemcitabine (20), and gemcitabine with cisplatin (21). It is anticipated that increased understanding about the molecular events involved in the development and progression of HCC will lead to more effective therapies. Evidence of the involvement of the MEK signaling pathway in hepatocarcinogenesis may lead to novel targeted therapies for HCC and research is on-going (22). Ex vivo assays that can accurately model in situ tumors would be an ideal platform for high through put screening of drug efficacy.
The purpose of this study was to test the feasibility of implementing a clinically relevant program that investigates individual patient’s tumors within the context of their care. We failed to grow tumors on three occasions despite finding viable tumor on conventional histology. We investigated several possible mechanisms including errors in processing or storage, tissue contamination, or the effects of concomitant medications such as antibiotics, immunosuppressants and anti-cancer agents. Close collaboration with the pathology department and relocation of the culture laboratory into the surgical area were used in response to the problems.
Although growing HCC in 3D culture has previously been demonstrated (23), here we have outlined the feasibility and potential for following a HCC patient cohort and comparing the phenotypic features of their HCC by histology and in 3DTC to their survival. Due to the limited number of patients in our study we were unable to test for correlations between the HCC phenotype, its growth in 3DTC, and their correlation to HCC recurrence or patient survival. Likewise we cannot comment on the impact of anticancer agents on 3DTC. However, we believe this experience has allowed us to establish a clinically relevant personalized research program that may eventually inform important clinical decisions. In addition we have found that 3DTC may be used to investigate fundamental questions such as the molecular biology of a cancer, or drug transport within the cancer, which may lead to care innovations. Finally, several of our patients were infected with hepatitis C virus or hepatitis B virus. The treatment of these viruses is species specific. We are attempting to adapt our 3DTC system to develop a human liver model of these infections in order to investigate novel approaches to treatment.
Tumor migration was inhibited by irinotecan, paclitaxel and docetaxel whereas the effect was inconsistent with 5FU and doxorubicin. Interestingly the latter two agents have been the mainstay of HCC treatment for over three decades. Paclitaxel and docetaxel are members of the taxane family of drugs, they are known to disrupt microtubule formation, an essential step in cell division. Irinotecan prevents DNA from unwinding. 3DTC may permit us to understand the specific intracellular pathways that are responsible for inhibition of HCC by these agents.
Chemotherapeutic agents are frequently used in combination protocols. It is possible that 5FU is more effective when used with other agents. This can be tested using the 3DTC model. While irinotecan and paclitaxel have also been used in combination protocols, they are rarely used together. By combining drugs we have arithmetically increased the options available for treatment. While increasing options seems beneficial, the possibility of determining the best protocol by randomized control trial is virtually impossible. 3DTC is amenable to testing many combinations on patient specific tissue. 3DTC may be a better method than animal research as a precursor to clinical trial.
Acknowledgements
None.
Footnote
Conflicts of Interest: Penny Costello and Warren McDonald hold patents for and have commercial interests in 3D in vitro culture assays. The remaining authors have no conflicts of interest to declare.
Ethical Statement: Approval for use of surgical specimens and collection of retrospective patient information was granted by the office of research ethics at the University of Western Ontario (REB number #11353E) and is in accordance with the declaration of Helsinki. Informed consent was gathered from each patient prior to surgery. Each patient willingly donated surgical specimens to this study.
References
- Mazzaferro V, Regalia E, Doci R, et al. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med 1996;334:693-9. [Crossref] [PubMed]
- Yao FY, Ferrell L, Bass NM, et al. Liver transplantation for hepatocellular carcinoma: expansion of the tumor size limits does not adversely impact survival. Hepatology 2001;33:1394-403. [Crossref] [PubMed]
- Parfitt JR, Marotta P, Alghamdi M, et al. Recurrent hepatocellular carcinoma after transplantation: use of a pathological score on explanted livers to predict recurrence. Liver Transpl 2007;13:543-51. [Crossref] [PubMed]
- Pineda-Solis K, McAlister V. Wading through the noise of “multi-omics” to identify prognostic biomarkers in hepatocellular carcinoma. Hepatobiliary Surg Nutr 2015;4:293-4. [PubMed]
- Miao R, Luo H, Zhou H, et al. Identification of prognostic biomarkers in hepatitis B virus-related hepatocellular carcinoma and stratification by integrative multi-omics analysis. J Hepatol 2014;61:840-9. [Crossref] [PubMed]
- Chen J, Liu J, Jin R, et al. Cytoplasmic and/or nuclear expression of β-catenin correlate with poor prognosis and unfavorable clinicopathological factors in hepatocellular carcinoma: a meta-analysis. PloS One 2014;9:e111885. [Crossref] [PubMed]
- Lin Y, Lin G, Fang W, et al. Increased expression of annexin A1 predicts poor prognosis in human hepatocellular carcinoma and enhances cell malignant phenotype. Med Oncol 2014;31:327. [Crossref] [PubMed]
- Wang J, Liu M, Chen L, et al. Overexpression of N-terminal kinase like gene promotes tumorigenicity of hepatocellular carcinoma by regulating cell cycle progression and cell motility. Oncotarget 2015;6:1618-30. [Crossref] [PubMed]
- Hashimoto R, Kanda M, Takami H, et al. Aberrant expression of melanoma-associated antigen-D2 serves as a prognostic indicator of hepatocellular carcinoma outcome following curative hepatectomy. Oncol Lett 2015;9:1201-6. [PubMed]
- Zheng X, Song T, Dou C, et al. CtBP2 is an independent prognostic marker that promotes GLI1 induced epithelial-mesenchymal transition in hepatocellular carcinoma. Oncotarget 2015;6:3752-69. [Crossref] [PubMed]
- Cukierman E, Pankov R, Stevens DR, et al. Taking cell-matrix adhesions to the third dimension. Science 2001;294:1708-12. [Crossref] [PubMed]
- Mizushima H, Wang X, Miyamoto S, et al. Integrin signal masks growth-promotion activity of HB-EGF in monolayer cell cultures. J Cell Sci 2009;122:4277-86. [Crossref] [PubMed]
- Antoni D, Burckel H, Josset E, et al. Three-dimensional cell culture: a breakthrough in vivo. Int J Mol Sci 2015;16:5517-27. [Crossref] [PubMed]
- Yoshii Y, Furukawa T, Waki A, et al. High-throughput screening with nanoimprinting 3D culture for efficient drug development by mimicking the tumor environment. Biomaterials 2015;51:278-89. [Crossref] [PubMed]
- Bauman GS, MacDonald W, Moore E, et al. Effects of radiation on a model of malignant glioma invasion. J Neurooncol 1999;44:223-31. [Crossref] [PubMed]
- Troussard AA, Costello P, Yoganathan TN, et al. The integrin linked kinase (ILK) induces an invasive phenotype via AP-1 transcription factor-dependent upregulation of matrix metalloproteinase 9 (MMP-9). Oncogene 2000;19:5444-52. [Crossref] [PubMed]
- Llovet JM, Ricci S, Mazzaferro V, et al. Sorafenib in advanced hepatocellular carcinoma. N Engl J Med 2008;359:378-90. [Crossref] [PubMed]
- Boige V, Raoul JL, Pignon JP, et al. Multicentre phase II trial of capecitabine plus oxaliplatin (XELOX) in patients with advanced hepatocellular carcinoma: FFCD 03-03 trial. Br J Cancer 2007;97:862-7. [PubMed]
- Gish RG, Porta C, Lazar L, et al. Phase III randomized controlled trial comparing the survival of patients with unresectable hepatocellular carcinoma treated with nolatrexed or doxorubicin. J Clin Oncol 2007;25:3069-75. [Crossref] [PubMed]
- Louafi S, Boige V, Ducreux M, et al. Gemcitabine plus oxaliplatin (GEMOX) in patients with advanced hepatocellular carcinoma (HCC): results of a phase II study. Cancer 2007;109:1384-90. [Crossref] [PubMed]
- Parikh PM, Fuloria J, Babu G, et al. A phase II study of gemcitabine and cisplatin in patients with advanced hepatocellular carcinoma. Trop Gastroenterol 2005;26:115-8. [PubMed]
- Facciorusso A, Licinio R, Carr BI, et al. MEK 1/2 inhibitors in the treatment of hepatocellular carcinoma. Expert Rev Gastroenterol Hepatol 2015;9:993-1003. [Crossref] [PubMed]
- Nakagawa T, Takahashi H, Kamiyama T, et al. In vitro chemosensitivity test for hepatocellular carcinoma using collagen-gel droplet embedded cultures. Gan To Kagaku Ryoho 2004;31:2145-9. [PubMed]


