Laparoscopic long sleeve pancreaticogastrostomy (LPG): a novel pancreatic anastomosis following central pancreatectomy
Introduction
Central pancreatectomy (CP) is preferred to distal pancreatectomy (DP) for patients with benign or neuroendocrine tumours located at the neck or distal body of the pancreas without vascular involvement, in order to preserve pancreatic parenchyma. Laparoscopic surgery is becoming more established in HPB surgery. However, following CP, pancreatic reconstruction of the pancreatic stump is difficult due to a soft pancreatic body and a normal, non-dilated pancreatic duct, leading to increased rates of postoperative pancreatic fistula (POPF). Conventional reconstructive techniques are either by pancreaticojejunostomy (1), with a Roux-en-Y loop anastomosis to either the end or side of the jejunum, or a pancreaticogastrostomy (PG) to the posterior wall of the stomach. For laparoscopic PJ, the formation of a Roux-en-Y loop has to be performed first before the pancreatic anastomosis, which is a technically challenging step that is also time-consuming. PG presents even further technical difficulties laparoscopically, as the pancreatic stump needs to be mobilised off the splenic vein for at least 4 cm in length before it can be safely reconstructed into the posterior wall of stomach. The latter requires an invagination of the pancreatic stump through gastrostomy in the posterior wall of stomach. It is extremely technically demanding to do this in a limited space and operative field laparoscopically.
In our centre, a novel technique has been described by a senior surgeon (Long R. Jiao), termed the laparoscopic long sleeve pancreaticogastrostomy (LPG) technique, a new laparoscopic method for reconstruction of the pancreatic stump during CP. It is envisaged that this technique avoids some of the technical challenges surrounding current methods of pancreatic stump anastomosis, without any increase in morbidity associated with the reconstruction. This may allow a greater proportion of surgeons to consider CP for appropriate patients.
Methods
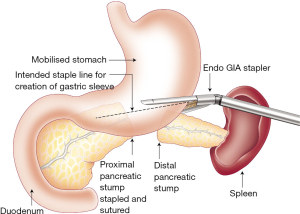
The LPG is performed by one senior HPB surgeon (Long R. Jiao). With the patient in a Lloyd-Davies position, laparoscopic CP is carried out using a standard five port technique (one camera and 4 mm × 10 mm ports). In brief, the procedure starts with incision of the gastrocolic omentum to access the lesser sac and expose the pancreas. Following evaluation of the anatomy, an intraoperative laparoscopic ultrasound of the pancreas is performed to confirm the location of the lesion. Next, the posterior peritoneum is incised at the inferior and superior margins of the pancreas to further expose the segment of the pancreas for resection. The distal resection margin is identified, formed by the course of the superior mesenteric vein (SMV) posterior to the pancreas. Next, the splenic artery is identified superior to the pancreas and slung using a vessel loop. A tunnel is created by dissecting posterior to the pancreas over the SMV, with careful ligation of the small pancreatic veins by a combination of LigaSure (Covidien, Hampshire, UK) and LigaClips (Ethicon, Berkshire, UK). Following this, the splenic vein is identified and dissected off the posterior pancreas. The proximal transection at the neck is then carried out using an EndoGIA laparoscopic stapling device (45 mm, blue cartridge; Covidien, Hampshire, UK) and the pancreatic stump oversewn with interrupted 2/0 prolene sutures. The pancreas dissection is continued towards the tail aided by traction sutures on the pancreas. Following adequate dissection 2 cm away from the tumour, the distal resection margin at the body/tail is transected using a combination of laparoscopic scissors and cautery.
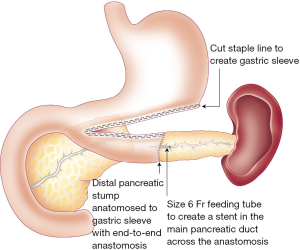
For the LPG, the pancreatic stump at body/tail is mobilized laparoscopically to free it at least 1 cm away from the splenic vein. The stomach is then brought down to measure and decide the position of LPG. A window is created at the point for gastroplasty in an avascular area of greater curvature of stomach. The gastroepiploic pedicle at this point is ligated with Hem-o-lok (Teleflex, NC, USA) and divided with laparoscopic scissors. Vertical band gastroplasty is then created with a 60mm EndoGIA stapler (TriStaple™, tan cartridge; Covidien, Hampshire, UK) over 3 cm away from the lesser gastric border to ensure gastric outlet patency (Figure 1). A long sleeve gastric tube measuring at least 6 cm in length in the greater curvature of stomach is then prepared and made ready for an end to end PG (Figures 1,2). A pancreatic stent is inserted into the pancreatic duct across the anastomosis whenever pancreatic duct is visible (Figure 2). A continuous running suture with 2/0 PDS is applied laparoscopically to the posterior wall and interrupted sutures to the anterior wall for an end-to-end LPG.
At the end of operation, a size 20 French Robinson drain is placed behind the anastomosis and the resected specimen is retrieved using an Endopouch specimen retrieval bag (Ethicon, Berkshire, UK), via either a Pfannenstiel incision or extension of the umbilical port incision, depending on the size of specimen.
Post-operatively patients are cared for on our hepatobiliary surgical ward with the introduction of clear fluids on day one and solid diet on day 3 as tolerated. Following discharge, patients are followed-up in the outpatient clinic 2 weeks post-operatively and then at three monthly intervals for the first year.
Results
Four patients underwent a laparoscopic CP using the LPG technique. There were 2 males and 2 females with a median age of 49 years (range, 30–65 years). All operations were completed laparoscopically with a mean operative time of 238.5±19.8 min. The length of time for reconstruction of LPG anastomosis was 37.6±7.6 min on average. Median length of stay was 5.5 days (range, 3.0–8.0 days). Final histology of these 4 cases revealed a side-branch IPMN with PanIN 2 (n=1), NET (n=1), metastatic melanoma (n=1) and MCN (n=1). Median tumour size was 23.4 mm (range, 28.3–30.0 mm). Median follow-up was 6.9 months (range, 2.0–18.0 months) with no mortality. One patient had a grade A POPF, as defined by the International Study Group on Pancreatic Fistula in 2005 (2). He had a high amylase level in the drain fluid (drained <30 mLs/24 hours), but was clinically well and was discharged with the drain in situ on the fifth post-operative day. The drain was removed 7 days after discharge in the outpatient clinic.
Discussion
CP was first described by Dagradi and Serio in 1984 and has since gained popularity amongst pancreatic surgeons. It has a lower risk of endocrine insufficiency and exocrine insufficiency than the alternative operation—DP (3-5). Laparoscopic central, rather than distal, pancreatectomy should be the operation of choice, when possible, for patients with benign or low-malignant pancreatic tumours at the neck or distal body of the pancreas to ensure pancreatic parenchymal and splenic preservation. However, worldwide there are few published reports on laparoscopic or robotic CP, with less than 40 cases in total and the largest series reporting only 11 cases (6-16) due to technical difficulties. We describe 4 cases of laparoscopic CP here with a novel reconstruction technique for the pancreatic stump. Laparoscopic LPG is a technically less demanding anastomosis, requiring just over half an hour of operative time in this series. There were no mortalities in our series, and one patient developed a grade A POPF, which was managed conservatively. In this case, the pancreatic duct could not be identified, nor stented intraoperatively. We have shown that the LPG technique is feasible with minimal morbidity. It may be technically easier to perform than conventional anastomotic methods. A randomized controlled trial is required to evaluate its operative outcomes, morbidity and mortality compared to current techniques.
Acknowledgements
We are grateful to Alliance Family Foundation for its support.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by institutional ethics board and informed consent was obtained from all patients.
References
- Kämpjärvi K, Mäkinen N, Kilpivaara O, et al. Somatic MED12 mutations in uterine leiomyosarcoma and colorectal cancer. Br J Cancer 2012;107:1761-5. [Crossref] [PubMed]
- Bassi C, Dervenis C, Butturini G, et al. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery 2005;138:8-13. [Crossref] [PubMed]
- Iacono C, Verlato G, Ruzzenente A, et al. Systematic review of central pancreatectomy and meta-analysis of central versus distal pancreatectomy. Br J Surg 2013;100:873-85. [Crossref] [PubMed]
- DiNorcia J, Ahmed L, Lee MK, et al. Better preservation of endocrine function after central versus distal pancreatectomy for mid-gland lesions. Surgery 2010;148:1247-54; discussion 1254-6. [Crossref] [PubMed]
- Xu SB, Zhu YP, Zhou W, et al. Patients get more long-term benefit from central pancreatectomy than distal resection: a meta-analysis. Eur J Surg Oncol 2013;39:567-74. [Crossref] [PubMed]
- Ayav A, Bresler L, Brunaud L, et al. Laparoscopic approach for solitary insulinoma: a multicentre study. Langenbecks Arch Surg 2005;390:134-40. [Crossref] [PubMed]
- DiNorcia J, Lee MK, Reavey PL, et al. One hundred thirty resections for pancreatic neuroendocrine tumor: evaluating the impact of minimally invasive and parenchyma-sparing techniques. J Gastrointest Surg 2010;14:1536-46. [Crossref] [PubMed]
- Giulianotti PC, Sbrana F, Bianco FM, et al. Robot-assisted laparoscopic middle pancreatectomy. J Laparoendosc Adv Surg Tech A 2010;20:135-9. [Crossref] [PubMed]
- Kang CM, Kim DH, Lee WJ, et al. Initial experiences using robot-assisted central pancreatectomy with pancreaticogastrostomy: a potential way to advanced laparoscopic pancreatectomy. Surg Endosc 2011;25:1101-6. [Crossref] [PubMed]
- Orsenigo E, Baccari P, Bissolotti G, et al. Laparoscopic central pancreatectomy. Am J Surg 2006;191:549-52. [Crossref] [PubMed]
- Boggi U, Amorese G, De Lio N, et al. Central pancreatectomy with inframesocolic pancreatojejunostomy. Langenbecks Arch Surg 2012;397:1013-21. [Crossref] [PubMed]
- Hong D, Xin Y, Cai X, et al. Application of binding pancreatogastrostomy in laparoscopic central pancreatectomy. World J Surg Oncol 2012;10:223. [Crossref] [PubMed]
- Sa Cunha A, Rault A, Beau C, et al. Laparoscopic central pancreatectomy: single institution experience of 6 patients. Surgery 2007;142:405-9. [Crossref] [PubMed]
- Zureikat AH, Nguyen KT, Bartlett DL, et al. Robotic-assisted major pancreatic resection and reconstruction. Arch Surg 2011;146:256-61. [Crossref] [PubMed]
- Sucandy I, Pfeifer CC, Sheldon DG. Laparoscopic assisted central pancreatectomy with pancreaticogastrostomy reconstruction - An alternative surgical technique for central pancreatic mass resection. N Am J Med Sci 2010;2:438-41. [Crossref] [PubMed]
- Abood GJ, Can MF, Daouadi M, et al. Robotic-assisted minimally invasive central pancreatectomy: technique and outcomes. J Gastrointest Surg 2013;17:1002-8. [Crossref] [PubMed]


