Societal reintegration following cadaveric orthotopic liver transplantation
Introduction
The only effective therapy for patients with end-stage liver disease (ESLD) is orthotopic liver transplantation (OLT). Since OLT was first performed in 1963 (1), advances in patient selection, operative techniques, anaesthesia and immunosuppression have significantly improved the success of the procedure with current survival rates of 74% at 5 years (2-4). In addition to survival benefits, OLT improves recipients’ quality of life (5-7). Despite these achievements, OLT remains a resource-intense therapy that has not been unanimously accepted as cost-effective (8-11). Cost-analysis studies tend to capture the expenses incurred around the time of admission for OLT but often fail to capture the costs related to failing to receive a transplant and succumbing to ESLD (12). Given the high costs of OLT, studies on the life experiences of OLT recipients may provide a better understanding of the value of the overall long-term effects of patients’ survival upon society (13). In fact, employment and societal reintegration of patients after OLT is not only a marker of clinically significant health recovery, but also an indirect means for society to recoup some of the resources that were expended in its support of transplantation activities.
Reintegration is a concept derived from criminal reform. Since its conceptualization it has been widely applied to health care as a metric to evaluate the success of a given intervention (14-17). Within the fields of traumatic brain injury, stroke, and trauma reintegration is a well-reported marker of successful outcomes. Within the field of solid organ transplantation, however, this data is limited. To better understand these issues, we performed a prospective surveillance study from a retrospectively identified cohort to determine whether OLT recipients at our center were able to return to their pre-operative marital status, employment status, if there were economical benefits for their families due to their better health status post-OLT, and if there were barriers that prevented them from becoming an integral part of their families and communities after being discharged from the hospital.
Methods
Patient population
Among 157 eligible candidates, 110 patients were followed in our prospective cohort study between September 2006 and January 2008. Due to the design, the number of patients enrolled in this study was fixed. The protocol and original data are available from the corresponding author. Patients enrolled in the study were identified retrospectively and were followed prospectively by the Multi-Organ Transplant Program (MOTP) at the Queen Elizabeth II Health Sciences Centre (QEIIHSC) in Halifax, Nova Scotia, Canada. The QEIIHSC is a tertiary teaching hospital affiliated with Dalhousie University. The MOTP is the only solid organ transplant program serving the Atlantic Provinces of Nova Scotia, Prince Edward Island, New Brunswick, Newfoundland and Labrador with a catchment population of approximately 2.3 million people.
To be included in this study, patients must have undergone cadaveric OLT at our institution at least 36 months prior to September 2006, be older than 18 years of age, able to provide verbal or written consent, in stable medical conditions for at least 2 weeks before recruitment, and without significant visual, hearing or other neurological impairments that could interfere with their cognitive function. A minimum period of 36 months after OLT was selected as an inclusion criteria based on previous studies that have shown that the likelihood of a complete recovery and physical ability to complete moderate physical tasks is optimized around the third postoperative year. Any patient with the presence of chronic liver graft rejection, liver dysfunction secondary to recurrent disease, history of longstanding non-compliance with immunosuppression medications, history of psychiatric disorder or illiteracy were excluded for they were considered at high risk of requiring multiple follow-ups in outpatient clinics or readmissions to the hospital, or other interventions that could interfere with their ability to be employed or reach their full potential as members of their communities.
Patient demographics and indications for OLT were retrieved from the MOTP digital database. Data reflecting socio-economic status, annual income, physical activity, and role satisfaction before and after OLT were captured by previously validated socio-economic instruments in the form of questionnaires that were completed via correspondence or at a scheduled follow-up appointment at our institution.
The primary aim of this study was to evaluate the rate of reintegration post-OLT in the specific domains of patients’ marital, employment, and financial roles. The secondary aims of this study were to determine the subjective role satisfaction and to identify any barriers to optimal functional reintegration.
This study was funded by a research grant from the Department of Surgery at Dalhousie University and was approved by the institutional ethic review board.
Instruments
The rate of societal reintegration in the domain of employment post-OLT was assessed using the self-administered Societal Reintegration Questionnaire (SRQ), a 6-item questionnaire instrument developed at Baylor University Medical Center (Dallas, USA) to assess patients’ involvement in a variety of activities following OLT (18). Questions addressed patients’ employment status and reasons for non-employment along with the number of hours spent per week on employment, home and/or household work, academic study, volunteer work and social and/or community group involvement. SRQ has shown content validity, test-retest reliability with Kappa coefficient of 0.67–1.0 for categorical responses and Pearson’s R correlation values of 0.8–0.99 for continuous values (14). SRQ was chosen as it has already been employed for similar studies with a high response rate of ≥90% of subjects (18).
The Work Productivity and Activity Impairment-General Health (WPAI-GH) Questionnaire was used to assess the hours absent from work due to health problems, the hours absent from work due to other reasons and the total number of hours actually worked during a determined period of time (19,20). The WPAI was developed to measure the effect of overall health and specific symptoms on productivity at work and personal life (21) and consists of six questions that elicit the following: employment status, hours missed because of specific health problems, hours missed because of other reasons, hour actually worked, the effect of the medical condition on the productivity while working, and the effect of the medical condition on the regular daily activities.
To improve the response rate, all eligible patients were sent an introductory letter to explain the aim and sponsorship of the survey, how respondents’ names were obtained, and the importance of their response and why a representative group was necessary for the validation of this study. The introductory letter was mailed out to all eligible subjects with a summary of the nature of the study and its rationale, emphasizing the confidentiality of the results and how the results would be used for academic purposes. Study subjects then called a toll-free or local phone number to express their interest in participating. A consent form was read to the subject on the phone and verbal consent was obtained. A telephone interview was then completed. A second envelope containing the signed consent form and the questionnaires with detailed instructions on how to complete them was sent to all the eligible subjects with a return pre-addressed and stamped envelope. A five-dollar gift certificate was enclosed with the questionnaires as an incentive to improve the participation rate.
To non-responders, two reminders were sent after the initial mailing of the introductory letter at three-week intervals. In addition, study coordinators made at least one phone call to all the non-responders who had a telephone number listed in our database or on the local directory list.
Data management
Data collected from the returned questionnaires were entered into a digital spreadsheet that was previously designed to mirror the sequence of questions mailed to the participants to minimize data entry errors. This study was funded by a research grant from the Department of Surgery at Dalhousie University. Cross analysis of random variables of the database was performed to assess potential transcription errors. If data entry errors were detected, the corresponding paper copy of the data collection form was retrieved and corrections made. A backup copy of the database was performed after each updating session. Confidentiality was protected by storing data in a secured location and by limiting data access to personnel responsible to update and collect the patients’ information and the primary investigators.
Definitions
Each patient was assigned to one of the six occupation groups listed below and each individual was assigned to only one group. If a patient was engaged in multiple activities, the subject was assigned to the profession where she/he spent the majority of her/his active time. The six occupation groups were: (I) low skill employment defined as having no more than a high school education and the majority of the job spent in physical or mechanical duties; (II) advanced skill employment included all the activities that required an education level beyond high school, good interpersonal skills, and high level of organization with the ability to work independently; (III) self employment was defined as any employment irrespective of education level whereby the individual was responsible for determining his or her own wages; (IV) disability was defined as the presence of any physical, sensory, cognitive or intellectual impairment that prevented participants from obtaining employment and required economic support by a funding agency (governmental or private institution); (V) housekeeping was defined as all the necessary activities for the good functioning of the household, supervision of any dependent member of the family, outdoor activities such as garden care, lawn and grounds maintenance, animal care and/or outbuilding maintenance; (VI) finally, retirement was defined as the cessation of any remunerated job due to age limitations or a decision to end one’s professional career.
Income included the sum of all the wages, salaries, profits, interest payments, rents and other forms of earnings received by the participants or their households in one year. Participants were asked to report the average personal or household income flow during the 5 years period before undergoing OLT and then the current incomes at the moment of enrolment in this study. No adjustment on reported incomes was performed to determine variation of the value of money over time due to inflation or interest rates changes. All reported incomes were calculated in Canadian dollars (CAN$) with exchange rate between CAN$ and USA dollar (US$) at 1:0.98 as of March 24th 2008.
Statistical analysis
Paired categorical variables were analyzed by McNemar Chi-Square or Fisher’s exact test and continuous variables by Student’s t-test. Non-paired categorical variables were analyzed by Chi-Square. For non-normally distributed parameters, Wilcoxon rank sum, Mann-Whitney, or Kruskal-Wallis test were employed. Two-tail tests with P values equal or less than 0.05 was considered statistical significant. All the statistical analyses were performed by using SPSS® version 20.0 (Chicago, Illinois, USA) software.
Results
Socio-demographic status
Among the 178 eligible patients who were alive at three years post-OLT at our center, 157 (88.2%) were candidates for this study and 110 (70%) participated by returning their questionnaires. Among the 21 excluded individuals, 15 were lost at follow up, 4 had developed cognitive impairment not recognized at the time of our screening for inclusion and exclusion criteria, and 3 had recurrent hepatic disease identified after their inclusion.
The demographic characteristics of all respondents are summarized in Table 1. The mean age of the patient population was 56 years and 43% were female with an average interval between the date of OLT and study enrolment of 8.7 years (SD 4.2).
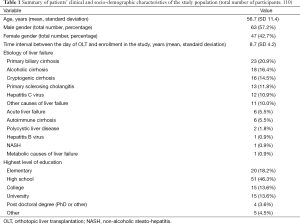
Full table
The main indication for OLT was ESLD due to autoimmune disorders (38.8%) such as primary biliary cirrhosis (20.9% of all cases), primary sclerosing cholangitis (11.8%) and autoimmune hepatitis (5.5%). Other significant causes of ESLD were alcoholic induced cirrhosis (16.4%) and viral hepatitis C (10.9%). High-school diploma had been obtained by 81.8% of patients, and of those, 16.7% went onto complete a college diploma and 26.7% went onto complete degrees from University or higher institutions.
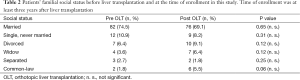
Prior to OLT, 75% of patients were married, 11% were single, 6% divorced, 4% widowed, and 1.8% were living with a common-law partner. Among the 12 participants who were single before OLT, two patients went onto become married and another lived with a common-law partner after surgery. Following OLT, 74.6% of the participants lived in a stable relationship with 69% married to the same spouse and 5.5% in a long-term relationship with their common-law partners. After undergoing OLT, eight participants became widowed and five divorced. The divorce rate increased from 6.4% to 9.1% while the percentage of single participants decreased from 10.9% to 8.2% following OLT (Table 2). The overall social status of patients undergoing OLT remained overall stable with 85.5% of patients living in the same social nucleus as prior to surgery.
Full table
Employment status
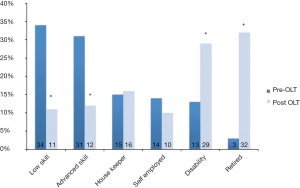
The employment status of the study population pre and post-OLT is shown in Figure 1. Before undergoing OLT, 71.9% of patients were employed and the remaining patients were housekeepers (13.6%), on disability (11.8%), or retired (2.7%). Among the participants who had employment, 43.1% were employed in low-skill activities, 39.2% in advanced-skill positions and 17.7% were self-employed. After OLT, the employment rate dropped to 30% and the disability rate increased from 11.8% to 26.4% (P=0.01). Similarly, the rate of retirement increased from 2.7% to 29.1% (P<0.01). Across all the categories of individuals working in low-skill, advanced-skill, or self-employed roles there was a significant decline in the number of individuals who were employed post-OLT (Figure 2).
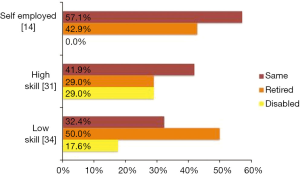
The percentage of individuals who returned to the same level of employment was proportional to the skill levels and the nature of the job as 57.1% of the self-employed workers, were able to return to the same level of employment, while 42.9% went onto retire and none went onto disability status. For advanced-skill workers, 41.9% were able to return to the same level of employment, while 29% went onto retire and 29% went onto disability. For low-skilled workers, 32.4% were able to return to the same level of employment, while 50% retired, and 17.6% went onto disability status (likelihood ratio P=0.04). All patients who were disabled prior to surgery remained on disability after undergoing OLT.
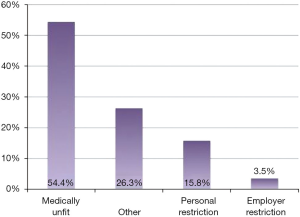
Overall, a total of 57 (51.8%) patients were unable to return to the same level of employment following OLT (Figure 3). Of these patients 54.4% were deemed medically unfit while 15.8% placed personal restrictions on their activity, and 3.5% were deemed unfit for work by their employer.
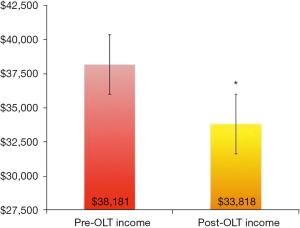
Income and societal role
Personal mean income/year of patients undergoing OLT was CAN$38,181 (SD 26,688) prior to OLT and decreased to CAN$33,818 (SD 26,946) at the time of enrolment with an average loss of CAN$4,363 (SD 20,733) (P=0.03) that corresponded to a correlation value of 0.7, suggesting that patients were likely to keep their earning rank (Figure 4), and patients in a higher income group before OLT were likely to remain in a higher earning bracket after surgery. Following OLT, 38% of patients reported improved earning potential due to their restored health. On the other hand, 21.3% of patients described at least one period of financial restriction requiring them to borrow money. Of these, 35% (7.3% overall) reported that they had experienced a financial crisis so severe that it temporarily compromised their ability to access immunosuppressive and other medications that were not completely covered by their health insurances.
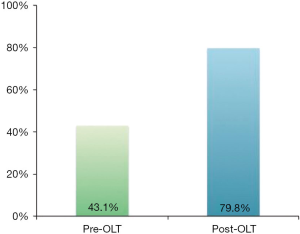
Among 110 participants, 88 (79.8%) responded that after undergoing OLT, they were pleased with their overall role in their communities and society in general (Figure 5).
Discussion
OLT is one of the most resource-intensive treatments for patients with end stage liver diseases. Not uncommonly, inpatient hospital charges exceed US$100,000 per transplant in the USA (22-24). Even in high-income societies where OLT is routinely performed, its cost-effectiveness has been questioned (25). For example, as a cost-saving measure in late 2010, OLT was temporarily removed from the benefits of Arizona Medicaid patients with hepatitis C (26). Even if this decision was subsequently revoked, it highlighted the issue that some treatments, although successful, might be too burdensome from a societal point of view. Therefore, an accurate assessment of factors affecting the costs of transplantation is important, not only to determine the financial costs incurred by the providers of transplant services, but also the economic costs borne by society and individual patients.
To fully analyze cost-effectiveness, the impact of restored health on care-giver burden and economic reintegration must be considered. While performing OLT for patients with decompensated ESLD is associated with high costs, the indirect costs of patients’ missed working days, hospitalizations, time off work for care-givers, expenses associated with procedures and medications necessary to control their disease etc. are included, then OLT might become the most desirable choice not only for patients survival, but also for the point of view of health-economics (27). From a health economics perspective, it is important that OLT recipients demonstrate some ability to return not only to a better health status, but also to an economically productive role. This could mitigate some of the criticism associated with the high upfront costs associated with OLT.
It has been previously reported that differences in disease etiology may affect return to employment rates (28). A systematic review in 2001 found that patients with alcohol induced cirrhosis were less likely to return to work than those with other etiologies, 33% and 80% respectively (29). These results were not confirmed in our study as we were underpowered to detect this. In our study, the overall employment rate fell from 72% pre-OLT to 30% post OLT (P=0.03) while the disability rate increased from 11.8% to 26.4% (P=0.01) and the rate of retirement increased from 2.7% to 29.1% (P<0.01). In the study by Bravata et al., the high rate of return to employment among non-alcohol cirrhotics could be attributed to a younger mean age of 44 compared to 56 in our study population. Another possible explanation for the low post-OLT employment rate observed in our study might have been due to the high proportion of patients (64%) who had low education levels (elementary and high school degree) and who had jobs where intense physical activity was required (e.g., farmers, fishermen, forestry workers etc.). Our results were more in keeping with the data reported in a recent analysis of 21,942 patients identified in the United Network for Organ Sharing Database by Huda et al. (30). In this study, the post-OLT employment rate was 24%. Upon multivariate analysis, younger age (18–40 years), male sex, college degree, Caucasian race and pre-transplant employment were positive predictors for patients’ employment after surgery.
Additional factors including, poor health, disability status, early retirement, and fear of losing disability benefits have been shown to be associated with unemployment post-OLT (31,32). However, in our study, despite the fact that patients expressed the desire to return to work, a proportion of patients (26%) were unable to do so as their positions were no longer available. The majority of patients who unable to return to work (54%) were told that they were unfit to return to their pre-transplant positions. For patients working in low-skill jobs, it is not infrequent that their positions are filled during the period when they are unwell and unable to work around the time of their OLT. In our cohort, the majority of patients who lost employment were in the categories of low skill jobs and went on to retire or apply for disability. On the other hand, 57% of self-employed individuals were able to return to their pre-OLT activities. For the entire cohort, age and job type were the strongest predictors of retirement while pre-op income was the strongest predictor of post-op disability status.
Following OLT the mean income among recipients dropped by 11% (mean $4,363; SD 20,733) (P=0.03) and 21% of patients reported at least one financial crisis when money had to be borrowed and 7.3% reported at least one severe financial crisis that impaired their ability to access medications including their immunosuppressive drugs. In the Canadian health care system each province is responsible for the provision of health resources and provincial pharmacare programs provide significant support for patients who need expensive medications. Therefore, it would be interesting to investigate the nature of other family expenditures that pushed immunosuppressant medications outside of the household budget, but that was not one of the aims of our study.
One of the most important findings of this study is that the majority of patients remained in the same familial nucleus and that 79% reported a significantly improved societal role satisfaction post-OLT despite their difficulties in returning to their pre-OLT jobs and the fact that they had an appreciable decline in their household incomes. Previous studies have shown that societal role satisfaction is strongly linked to health related quality of life and according to Cowling et al., there are significant differences in how men and women perceive quality of life post-OLT (33,34). These results are affected by both education and employment status. Among highly educated recipients, men reported higher quality of life than women, despite similar rates of employment. This is in keeping with studies that suggest women demonstrate more psychological distress as a direct result from the traditional societal roles they often occupy (33,35).
As part of a multi-disciplinary assessment, the OLT candidates at our institution undergo a pre-operative assessment by physicians, nurse coordinators, nutritionists, physical therapists, psychologists and social workers. This assessment is tailored to each patient with respect to the number and duration of sessions. Among other things, the patient’s living arrangements, family supports, employment, income, and community supports are evaluated and, following the assessment, interventions in the form of counselling or facilitating community supports are arranged. Our multidisciplinary team is also available for patients who require post-OLT support. Typically these sessions focus on psycho-social issues such as “survivor guilt”, post-traumatic stress, anxiety, depression, and poor sexual function. We have shown here that economic reintegration should also be a focus of both pre- and post-OLT counseling. One of the possible interventions targeting these challenges might be the need to educate both our patients and their employers that after OLT, patients should be able to return to their jobs unless unexpected complications occur preventing their full reintegration. Ideally, parallel to the medical and psychosocial rehabilitation that is already available in most transplant centers, patients should be offered a vocational rehabilitation program similar to what is already in place for military personnel who return to civilian life. In these programs, vocational professionals assist individuals to transfer their skills and education into rewarding professional careers by identifying suitable jobs, by providing career finding services (such as resume writing and interview skills) and financial support for training and related costs such as tuitions and books. To the best of our knowledge, there are no studies that have assessed the financial impact of vocational rehabilitation programs for recipients of liver transplants. However, the measurement of cost-effectiveness has become imperative in this era of scarce resources and the hypothesis that participation in supported employment programs improves reintegration should be explored in future studies. It is likely that vocational rehabilitation would directly result in improved incomes for patients and thus indirectly result in lower overall economic burden for society (36).
There are several weaknesses of this study including the overall small number of patients who were recruited in a single center, the fact that patients had to recall some of the variables such as their pre-OLT incomes and societal satisfaction, and the fact that the instruments used were completed by patients and data could not be verified by the investigators for accuracy. Therefore, recollection and reporting bias might have contributed to the differences noted between our results and data from previous studies.
Another important limitation is that our study population might be significantly different from recipients who undergo OLT in other programs. In fact, the population living in the four Atlantic Canadian provinces served by our transplant program, is predominantly of Caucasian descent, has a lower educational level, higher disability rate, and lower overall income in comparison to the rest of the Canadian population. Among our patients, the rate of autoimmune liver failure was much higher than internationally reported data. At our institution, primary biliary cirrhosis represented 20.9% of cases, primary sclerosing cholangitis 11.8%, and autoimmune hepatitis 5.5%. Other significant causes of ESLD were alcoholic cirrhosis in 16.4% of participants and hepatitis C virus (HCV) in 10.9%. Among the United Network for Organ Sharing database from 1994–2009 nearly 50% of transplants were performed for alcoholic and HCV cirrhosis (37). Despite these differences, we think that our data are still applicable to the broader population of OLT patients.
Conclusions
Following OLT, the vast majority of patients in this study were reintegrated in their familiar nucleus but only a minority was able to return to the employment positions held before surgery. This resulted in reduced incomes that were significant enough to limit access to immunosuppressant medications for short periods of time. Despite these financial drawbacks, the majority of recipients reported improved societal role satisfaction after surgery. Our findings suggest that in our population, one of the most effective strategies to assist patients with ESLD should focus on maintaining their professional abilities while on the waiting list, and to assist them to transition to their professional roles after OLT. These policies would not only improve patients’ and their families’ financial status, but also increase the overall societal benefits provided by OLT.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was approved by the institutional ethic review board and informed consent was obtained from all patients.
References
- Starzl TE, Marchioro TL, Vonkaulla KN, et al. Homotransplantation of the liver in humans. Surg Gynecol Obstet 1963;117:659-76. [PubMed]
- Lipshutz GS, Hiatt J, Ghobrial RM, et al. Outcome of liver transplantation in septuagenarians: a single-center experience. Arch Surg 2007;142:775-81; discussion 781-4. [Crossref] [PubMed]
- Canadian Institute for Health Information (CIHI) 2015 Compairing the Canadian Organ Replacement Registry (CORR) Report: Treatment of End-Stage Organ Failure in Canada (2004-2013). Available online: https://secure.cihi.ca/estore/productFamily.htm?locale=en&pf=PFC2864&lang=en
- 2003 U.S. Organ Procurement and Transplantation Network (OPTN) and the Scientific Registry of Transplant Recipients (SSTR) Annual Report. Available online: http://www.srtr.org/annual_reports/archives/2003/2003_Annual_Report/
- Moore DE, Feurer ID, Speroff T, et al. Impact of donor, technical, and recipient risk factors on survival and quality of life after liver transplantation. Arch Surg 2005;140:273-7. [Crossref] [PubMed]
- Evans RW. Organ transplantation and the inevitable debate as to what constitutes a basic health care benefit. Clin Transpl 1993.359-91. [PubMed]
- Evans RW, Kitzmann DJ. Contracting for services: liver transplantation in the era of mismanaged care. Clin Liver Dis 1997;1:287-303. viii. [Crossref] [PubMed]
- Showstack J, Katz PP, Lake JR, et al. Resource utilization in liver transplantation: effects of patient characteristics and clinical practice. NIDDK Liver Transplantation Database Group. JAMA 1999;281:1381-6. [Crossref] [PubMed]
- Wiesner RH, Lombardero M, Lake JR, et al. Liver transplantation for end-stage alcoholic liver disease: an assessment of outcomes. Liver Transpl Surg 1997;3:231-9. [Crossref] [PubMed]
- Sagmeister M, Mullhaupt B, Kadry Z, et al. Cost-effectiveness of cadaveric and living-donor liver transplantation. Transplantation 2002;73:616-22. [Crossref] [PubMed]
- Taylor MC, Greig PD, Detsky AS, et al. Factors associated with the high cost of liver transplantation in adults. Can J Surg 2002;45:425-34. [PubMed]
- Wong LL, McFall P, Wong LM. The cost of dying of end-stage liver disease. Arch Intern Med 1997;157:1429-32. [Crossref] [PubMed]
- Williams JW, Vera S, Evans LS. Socioeconomic aspects of hepatic transplantation. Am J Gastroenterol 1987;82:1115-9. [PubMed]
- O'Neill J, Hibbard MR, Brown M, et al. The effect of employment on quality of life and community integration after traumatic brain injury. J Head Trauma Rehabil 1998;13:68-79. [Crossref] [PubMed]
- Fuhrer MJ, Rintala DH, Hart KA, et al. Relationship of life satisfaction to impairment, disability, and handicap among persons with spinal cord injury living in the community. Arch Phys Med Rehabil 1992;73:552-7. [PubMed]
- Trieschmann RB. Psychosocial research in spinal cord injury: the state of the art. Paraplegia 1992;30:58-60. [Crossref] [PubMed]
- Whiteneck GG, Charlifue SW, Gerhart KA, et al. Quantifying handicap: a new measure of long-term rehabilitation outcomes. Arch Phys Med Rehabil 1992;73:519-26. [PubMed]
- Cowling T, Jennings LW, Goldstein RM, et al. Societal reintegration after liver transplantation: findings in alcohol-related and non-alcohol-related transplant recipients. Ann Surg 2004;239:93-8. [Crossref] [PubMed]
- Goetzel RZ, Ozminkowski RJ, Long SR. Development and reliability analysis of the Work Productivity Short Inventory (WPSI) instrument measuring employee health and productivity. J Occup Environ Med 2003;45:743-62. [Crossref] [PubMed]
- Prasad M, Wahlqvist P, Shikiar R, et al. A review of self-report instruments measuring health-related work productivity: a patient-reported outcomes perspective. Pharmacoeconomics 2004;22:225-44. [Crossref] [PubMed]
- Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. Pharmacoeconomics 1993;4:353-65. [Crossref] [PubMed]
- Buchanan P, Dzebisashvili N, Lentine KL, et al. Liver transplantation cost in the model for end-stage liver disease era: looking beyond the transplant admission. Liver Transpl 2009;15:1270-7. [Crossref] [PubMed]
- Axelrod DA, Gheorghian A, Schnitzler MA, et al. The economic implications of broader sharing of liver allografts. Am J Transplant 2011;11:798-807. [Crossref] [PubMed]
- Axelrod DA, Koffron AJ, Baker T, et al. The economic impact of MELD on liver transplant centers. Am J Transplant 2005;5:2297-301. [Crossref] [PubMed]
- Axelrod DA. Economic and financial outcomes in transplantation: whose dime is it anyway? Curr Opin Organ Transplant 2013;18:222-8. [Crossref] [PubMed]
- Sack K. Arizona Medicaid cuts seen as a sign of the times. New York Times. 4 December 2010.
- Bajaj JS, Wade JB, Gibson DP, et al. The multi-dimensional burden of cirrhosis and hepatic encephalopathy on patients and caregivers. Am J Gastroenterol 2011;106:1646-53. [Crossref] [PubMed]
- Abosh D, Rosser B, Kaita K, et al. Outcomes following liver transplantation for patients with alcohol- versus nonalcohol-induced liver disease. Can J Gastroenterol 2000;14:851-5. [Crossref] [PubMed]
- Bravata DM, Olkin I, Barnato AE, et al. Employment and alcohol use after liver transplantation for alcoholic and nonalcoholic liver disease: a systematic review. Liver Transpl 2001;7:191-203. [Crossref] [PubMed]
- Huda A, Newcomer R, Harrington C, et al. High rate of unemployment after liver transplantation: analysis of the United Network for Organ Sharing database. Liver Transpl 2012;18:89-99. [Crossref] [PubMed]
- Hunt CM, Tart JS, Dowdy E, et al. Effect of orthotopic liver transplantation on employment and health status. Liver Transpl Surg 1996;2:148-53. [Crossref] [PubMed]
- Rongey C, Bambha K, Vanness D, et al. Employment and health insurance in long-term liver transplant recipients. Am J Transplant 2005;5:1901-8. [Crossref] [PubMed]
- Cowling T, Jennings LW, Goldstein RM, et al. Liver transplantation and health-related quality of life: scoring differences between men and women. Liver Transpl 2004;10:88-96. [Crossref] [PubMed]
- Painter P, Krasnoff J, Paul SM, et al. Physical activity and health-related quality of life in liver transplant recipients. Liver Transpl 2001;7:213-9. [Crossref] [PubMed]
- Gove WR. Gender differences in mental and physical illness: the effects of fixed roles and nurturant roles. Soc Sci Med 1984;19:77-91. [Crossref] [PubMed]
- Clark RE, Dain BJ, Xie H, et al. The economic benefits of supported employment for persons with mental illness. J Ment Health Policy Econ 1998;1:63-71. [Crossref] [PubMed]
- Singal AK, Guturu P, Hmoud B, et al. Evolving frequency and outcomes of liver transplantation based on etiology of liver disease. Transplantation 2013;95:755-60. [Crossref] [PubMed]


