
The global burden of fatty liver disease: the major impact of China
Due to the energy-dense but nutrient-deficient diets, sedentary lifestyle and lack of exercise as well as an aging population, the prevalence and incidence of overweight/obesity/sarcopenic obesity, type 2 diabetes mellitus (T2DM), metabolic syndrome and their related non-alcoholic fatty liver disease (NAFLD) have been increasing globally in the last two decades. In Europe and the United States, NAFLD has become the second leading cause of end-stage liver disease and liver transplantation (1). Worse still, the onset age of NAFLD is becoming younger tendency. Although the new nomenclature of metabolic dysfunction-associated fatty liver disease (MAFLD) has been proposed for 3 years, MAFLD is not equivalent to NAFLD, and few epidemiologic investigations on MAFLD to date. Therefore, this invited editorial is focus on the global epidemiology of NAFLD and the major impact on China.
Global epidemiology of NAFLD
Riazi et al. (2) conducted a systematic review and meta-analysis of 72 studies with a total of 1,030,160 respondents in 17 countries worldwide by May 25, 2021, and found that the overall global prevalence of NAFLD was estimated to be 32.4% [95% confidence interval (CI): 29.9–34.9%], significantly higher in men (39.7%) than women (25.6%). The overall NAFLD prevalence increased over time, from 25.5% in or before 2005 to 37.8% in 2016 or later. A meta-analysis from Younossi et al. (3) reported that the overall global prevalence of NAFLD was highest in Latin America (44.37%), followed by the Middle East and North Africa, South Asia, South-East Asia, North America, East Asia, and lowest in Western Europe (25.10%) (Figure 1A).
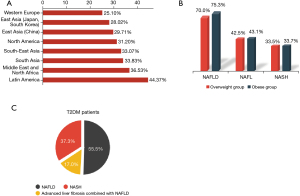
The systematic review and meta-analysis by Quek et al. (4) included 151 studies from 2000 to 2022 with 101,028 adults enrolled, which revealed that the prevalence rate of NAFLD, non-alcoholic fatty liver (NAFL), and non-alcoholic steatohepatitis (NASH) in the overweight group was 70.0%, 42.5% and 33.5%, respectively, and the rate was 75.3%, 43.1% and 33.7% among the obese group (Figure 1B); the proportion of significant fibrosis in overweight and obese patients with NAFLD was 20.3% and 21.6%, respectively, and the proportion of advanced fibrosis was 6.7% and 6.9%, respectively. Another meta-analysis by Younossi et al. (5) included 80 studies from 20 countries with a total of 49,419 patients with T2DM, and the results showed that the overall prevalence of NAFLD and NASH was 55.5% (95% CI: 47.3–63.7%) and 37.3% (95% CI: 24.7–50.0%), respectively; and the prevalence of advanced fibrosis was 17.0% (95% CI: 7.2–34.8%) in diabetic patients with NAFLD (Figure 1C).
A systematic review and meta-analysis by Le et al. (6) reported that the pooled incidence of NAFLD in Asian adults was 46.13/1,000 person-years (95% CI: 39.32–52.94); the incidence of NAFLD in men was significantly higher than that in women (53.10 vs. 33.70/1,000 person-years); the risk of NAFLD in obese or overweight/obese group was about three times higher than that in non-obese or normal body mass index (BMI) group (86.7 vs. 29.64 and 84.17 vs. 33.58/1,000 person-years). Further multiple regression analysis revealed that the research period and geographic location were independently associated with the incidence of NAFLD, and the incidence rate was highest in China (59.40/1,000 person-years) and lowest in Japan (23.20/1,000 person-years).
Epidemiology of NAFLD in China
China has a large population and uneven distribution, with obvious diversity in culture, geography, economy and lifestyle, which leads to some regional differences in the prevalence of NAFLD in Chinese. Details on the epidemiology of NAFLD/MAFLD in mainland China are shown in Table 1.
Table 1
| Study | Data source | Type of study | Study period | Total number | Prevalence | Prevalence of MAFLD |
|---|---|---|---|---|---|---|
| Zhou et al., 2020, (7) | Mainland China | Systematic review and meta-analysis | 1999–2018 | 1,030,160 | 29.6% (NAFLD) | – |
| Zeng et al., 2022, (8) | Chongming District, Shanghai, China | Community-based cross-sectional study | 2011–2012 | 9,927 (>40 years old) |
36.9% (NAFLD) | 40.3% |
| Zeng et al., 2023, (9) | Shanghai, China | Cohort study | 2017–2022 | 848 (8 years old) |
5.07% (FLD) | 3.42% |
| Man et al., 2023, (10) | Mainland China | Population-based, cross-sectional study | 2017–2022 | 5,757,335 | 44.39% (hepatic steatosis), 10.57% (severe steatosis), 2.85% (advanced fibrosis), 0.87% (cirrhosis) |
– |
NAFLD, non-alcoholic fatty liver disease; MAFLD, metabolic dysfunction-associated fatty liver disease; FLD, fatty liver disease.
According to the systematic review and meta-analysis by Zhou et al. (7), the overall prevalence of NAFLD in the past 20 years was 29.6% (95% CI: 28.2–31.0%), which was obviously higher in men (34.75%) than in women (23.50%). Although the prevalence increased with age (8.54% in 18–29 years old, 29.14% in 50–59 years old), it showed a downward trend in population aged after 70 years old (23.79%). Besides, the prevalence of NAFLD in patients with obesity and T2DM was as high as 66.21% and 51.83%, respectively. Also, the incidence of NAFLD has been increasing over time, from 4.2% (95% CI: 2.3–6.0%) during 2007–2010, 4.6% (95% CI: 3.3–6.0%) during 2011–2013 to 5.2% (95% CI: 3.9–6.5%) during 2014–2016. Nevertheless, there was a considerable heterogeneity in these results, and the majority of the studies were not from the general adult population in random cluster sampling.
Zeng et al. (8) reported a large sample of survey of T2DM and ultrasound-diagnosed fatty liver in a random cluster sampling of adults aged 40 years or older in Chongming District, Shanghai, China. The results demonstrated that the prevalence of NAFLD and MAFLD was 36.9% and 40.3% in 9,927 adults, respectively. A total of 3,481 (35.1%) patients met the diagnostic criteria for both MAFLD and NAFLD (MAFLD+NAFLD+), 521 (5.2%) patients were MAFLD alone, most of them with excessive alcohol intake, and 181 (1.8%) patients had NAFLD alone, of them 82.9% had a metabolic cardiovascular risk factor. In addition, the prevalence of NAFLD increased with the severity of impaired glucose metabolism, from 35.7% in impaired fasting glucose, 40.9% in impaired glucose tolerance, to 53.8% in T2DM patients. Therefore, the prevalence of MAFLD might be a little higher than NAFLD, and around 95.0% patients with NAFLD could be classified as MAFLD. According to the new definition of metabolic dysfunction-associated steatotic liver disease (MASLD), prevalence of MASLD seems to be higher than MAFLD as the majority of patients with NAFLD alone can be classified into MASLD, and almost all patients with alcoholic liver disease (ALD) also met both diagnostic criteria for MAFLD and MASLD (Met-ALD) (11).
Recently, Man et al. (10) retrospectively analyzed the big data of health checkups at Meinian Health Industry Company from 30 provinces in China from 2017–2022. Among 5,757,335 adults who had received liver transient elastography examination by FibroTouch®, the prevalence of hepatic steatosis [ultrasound attenuation parameter (UAP) >244 dB/m], severe steatosis (UAP >296 dB/m), advanced fibrosis [liver stiffness measurement (LSM) >10 kPa], and cirrhosis (LSM >13.5 kPa) were 44.39%, 10.57%, 2.85%, and 0.87%, respectively. The prevalence rates of various degrees of steatosis and fibrosis in the subgroups of males, obesity, diabetes mellitus, hypertension, dyslipidemia, metabolic syndrome, and increased serum alanine transaminase (ALT) or aspartate aminotransferase levels were significantly higher than those in the correspondent control group. Furthermore, the prevalence of liver fibrosis was considerably higher in the group with fatty liver, low blood albumin levels, or low platelet count, and hepatitis B virus (HBV) infection than in the control group. However, this study was not from a community or block randomized sample population, was approximately two-thirds male, and did not differentiate between ALD and NAFLD, making it impossible to calculate a sex- and age-adjusted prevalence of NAFLD in our general population.
Although there is a potentially negative association between chronic HBV infection and the prevalence of NAFLD in Chinese, the prevalence of NAFLD and MAFLD also increased with time in HBV infected patients (12). Prevalence (18.2%) of NASH in 1,000 patients with chronic hepatitis B and significant fibrosis before antiviral treatment was found to be 18.2%, and the resolution and incidence rate of NASH after 72-week entecavir treatment was 43.0% and 4.0%, respectively. Prevalence, resolution and incidence rate of NASH in these patients were related to overweight at baseline and subtle weight change during follow-up (13).
Pediatric NAFLD in China and Asia
A meta-analysis by Zou et al. (14) included nine studies from 33 Asian populations with a total of 20,595 children up to April 2021, and found that the overall prevalence of pediatric NAFLD was 5.53% (95% CI: 3.46–8.72%) with an increasing trend in the last decade, and 36.64% (95% CI: 27.99–46.26%) of children with ultrasound-based NAFLD had elevated serum ALT levels. In addition, prevalence of NAFLD in boys (8.18%, 95% CI: 4.93–13.26%) was higher than in girls (3.60%, 95% CI: 1.60–7.87%). After age 10, boys were more prone to develop NAFLD than girls (odds ratio =1.75; P=0.0012). Furthermore, the pooled prevalence of NAFLD was sequentially increased in normal weight (1.49%, 95% CI: 0.88–2.51%, n=2,610), overweight (16.72%, 95% CI: 7.07–34.65%, n=1,265), and obese children (50.13%, 95% CI: 41.99–58.27%, n=6,434). Multivariate meta-regression confirmed that boy proportion (P=0.0396) and BMI (P<0.0001) were positively associated with NAFLD prevalence. Recently, Zeng et al. (9) investigated 848 children aged 8 years (431 boys) from a Shanghai birth cohort study, of whom 385 children (189 boys) also had a 5-year follow-up. The results showed an increase in the prevalence of FLD from 3.9% at age 5 years to 5.07% at age 8 years, and an increase in the MAFLD prevalence from 0.52% to 3.42%.
In summary, NAFLD is an important chronic noncommunicable disease closely associated with overweight/obesity, T2DM, and metabolic syndrome, majority of them belong to MAFLD or MASLD. Given that MAFLD/MASLD can occur in patients with other liver diseases, the prevalence of MAFLD/MASLD is presumed to be significantly higher than that of NAFLD. Global incidence of NAFLD has been increasing over the past decades, especially in China. Despite its huge disease burden, NAFLD is being addressed only by emerging global public health campaigns, and it is absent from almost all national and international strategies and policies for noncommunicable diseases (15). If effective measures are not taken in time, the disease burden of NAFLD will continue to rise at an alarming rate in the future. It is critical for hepatologists to collaborate with other stakeholders to improve NAFLD care, bringing further strength and wisdom to the diagnosis and therapy of NAFLD.
Acknowledgments
Funding: This study was supported by
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Hepatobiliary Surgery and Nutrition. The article did not undergo external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://hbsn.amegroups.com/article/view/10.21037/hbsn-23-556/coif). The authors report that this study was supported by the National Natural Science Foundation of China (Nos. 82170593, 81900507). The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Devarbhavi H, Asrani SK, Arab JP, et al. Global burden of liver disease: 2023 update. J Hepatol 2023;79:516-37. [Crossref] [PubMed]
- Riazi K, Azhari H, Charette JH, et al. The prevalence and incidence of NAFLD worldwide: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol 2022;7:851-61. [Crossref] [PubMed]
- Younossi ZM, Golabi P, Paik JM, et al. The global epidemiology of nonalcoholic fatty liver disease (NAFLD) and nonalcoholic steatohepatitis (NASH): a systematic review. Hepatology 2023;77:1335-47. [Crossref] [PubMed]
- Quek J, Chan KE, Wong ZY, et al. Global prevalence of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis in the overweight and obese population: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol 2023;8:20-30. [Crossref] [PubMed]
- Younossi ZM, Golabi P, de Avila L, et al. The global epidemiology of NAFLD and NASH in patients with type 2 diabetes: A systematic review and meta-analysis. J Hepatol 2019;71:793-801. [Crossref] [PubMed]
- Le MH, Le DM, Baez TC, et al. Global incidence of non-alcoholic fatty liver disease: A systematic review and meta-analysis of 63 studies and 1,201,807 persons. J Hepatol 2023;79:287-95. [Crossref] [PubMed]
- Zhou J, Zhou F, Wang W, et al. Epidemiological Features of NAFLD From 1999 to 2018 in China. Hepatology 2020;71:1851-64. [Crossref] [PubMed]
- Zeng J, Qin L, Jin Q, et al. Prevalence and characteristics of MAFLD in Chinese adults aged 40 years or older: A community-based study. Hepatobiliary Pancreat Dis Int 2022;21:154-61. [Crossref] [PubMed]
- Zeng J, Jin Q, Yang J, et al. Prevalence and incidence of MAFLD and associated anthropometric parameters among prepubertal children of the Shanghai Birth Cohort. Hepatol Int 2023;17:1416-28. [Crossref] [PubMed]
- Man S, Deng Y, Ma Y, et al. Prevalence of Liver Steatosis and Fibrosis in the General Population and Various High-Risk Populations: A Nationwide Study With 5.7 Million Adults in China. Gastroenterology 2023;165:1025-40. [Crossref] [PubMed]
- Rinella ME, Lazarus JV, Ratziu V, et al. A multisociety Delphi consensus statement on new fatty liver disease nomenclature. Hepatology 2023;78:1966-86. [Crossref] [PubMed]
- Shi YW, Yang RX, Fan JG. Chronic hepatitis B infection with concomitant hepatic steatosis: Current evidence and opinion. World J Gastroenterol 2021;27:3971-83. [Crossref] [PubMed]
- Chang XJ, Shi YW, Wang J, et al. Influence of weight management on the prognosis of steatohepatitis in chronic hepatitis B patients during antiviral treatment. Hepatobiliary Pancreat Dis Int 2021;20:416-25. [Crossref] [PubMed]
- Zou ZY, Zeng J, Ren TY, et al. The burden and sexual dimorphism with nonalcoholic fatty liver disease in Asian children: A systematic review and meta-analysis. Liver Int 2022;42:1969-80. [Crossref] [PubMed]
- Lazarus JV, Mark HE, Anstee QM, et al. Advancing the global public health agenda for NAFLD: a consensus statement. Nat Rev Gastroenterol Hepatol 2022;19:60-78. [Crossref] [PubMed]


