
Alcohol-related liver disease
Among individuals with known alcohol use disorder (AUD), the prevalence of alcoholic fatty liver disease (AFLD) is present in 25–90% of cases (1). Shroff et al. (1) report that the annual progression to cirrhosis is 3% in the presence of AFLD, 10% in case of alcohol-related steatohepatitis (ASH) and 8% with any grade of pre-cirrhotic fibrosis. Alcohol-related liver disease (ALD) is the cause of 36% of cases of cirrhosis in the United States and nearly one half of cirrhosis-related deaths worldwide (1). Ethanol is a recognized carcinogen for several malignancies with the risk starting at low dose (10 gr/1 unit/day) (2). The link between alcohol consumption (AC) and hepatocellular carcinoma (HCC) is well known: various evaluations carried out by both USA and Italian groups indicate that such a correlation is present in 32% to 45% of cases (2). With the reduction of hepatitis C virus (HCV) cases, AC will become the main cause of HCC in Western countries. Furthermore, ALD and metabolic syndrome (MS) are currently the main causes of liver transplantation (LT) (3).
Recently, Parker et al. (4) raised, among many, some key points:
- Identify the presence of unknown AUD in a patient with liver disease.
- Identify the presence of liver fibrosis (LF) early.
- Manage ALD patients (especially in advanced cases) in the presence of an addiction specialist.
Regarding the first point, it is well known that hepatologists are underprepared to diagnose and treat AUD despite its high prevalence in patients with liver disease (1). The lag time between the occurrence of AUD and the first clinical detection may take years in daily practice, leading to a significant delay in the beginning of an intervention and potentially causing the undertreatment of this population (5). For this reason, it is strongly recommended to subject all patients with liver injury (LJ) to the alcohol use disorder identification test (AUDIT). This tool also highlights low risk AC and furthermore it was associated with mortality risk. However, it is only used in 10% of cases (5). AUDIT must also be used in the case of mild LJ and in any case regardless of the type of diagnosis (6). In fact, alcohol abstention improves the patient’s prognosis (hepatic and extrahepatic) and avoids possible drug interference. All scientific societies in the sector recommend nonalcoholic fatty liver disease (NAFLD)/metabolic associated fatty liver disease (MAFLD) patients not to consume alcoholic beverages (6).
Second point: the diagnosis of alcohol-related LF is often late.
ALD patients are often asymptomatic and with mild dysfunction. For this reason, European guidelines recommend using validated methods for early diagnosis and identification of patients at risk (7). It is known, in fact, that the diagnosis of ALD is often late and referral to an alcohol unit with hepatological expertise can be carried out with a delay of up to 40 months (8). This also happens in the Italian reality where alcohol screening is carried out only on a modest part of patients and where only a third of general practitioners (GPs) use the AUDIT or the short AUDIT (AUDIT-C) and practice the brief intervention.
More recently, in a cross-sectional analysis of patients with liver disease worldwide, Shah et al. (9) found that patients with ALD are seen with more advanced stage disease than patients with HCV-associated liver disease. Of patients with 2 etiologies of liver disease, excess alcohol use was associated with 50% of cases. It is necessary to identify subjects with LF early and subsequently subject them to personalized therapy to eliminate the etiological factors of liver injury through common international guidelines. Therefore, all patients with AUD should undergo initial access to ultrasonography (US) with elastography for early detection of LF or HCC.
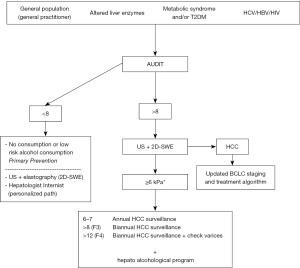
Figure 1 proposes a possible path according to the AUDIT and the degree of fibrosis. Fibrosis is the most significant predictor of both prognosis and long-term survival. Its identification helps to promote lifestyle changes (smoking cessation, alcohol abstention, proper nutrition, physical activity, etc.) and when cardiovascular (CV) and oncologic screening is necessary (6). Liver biopsy certainly represents the gold standard to diagnose and to stage LF, however, it is not routinely performed due to its invasive nature. Non-invasive methods have been proposed to identify and characterize LF. Some use direct markers that detect extracellular matrix turnover, and other indirect markers that indicate alterations in liver function. As reported in our previous papers, these methodologies report variable data and do not always represent a reliable tool for evaluating the LF degree.
Elastography is currently a tool that is easily used in accredited centers. Most studies report the experience of transient elastography (TE), however numerous confounding factors have been identified (inflammation-congestion, active AC, obesity, cholestasis, amyloidosis and, in some cases, inexperience) (6). Two-dimensional shear wave elastography (2D-SWE) is becoming an increasingly used and reliable technique. Correspondence was found between SWE, acoustic radiation force impulse (ARFI), TE and histological fibrosis score. However, some authors have reported greater accuracy of 2D-SWE compared to TE regarding advanced fibrosis (F3–F4) and better accuracy than ARFI for identification of significant fibrosis (10). Thiele et al. (10) in a biopsy-controlled study, included ALD patients who underwent enhanced LF, FibroTest, TE and 2D-SWE on the same day. Enhanced liver fibrosis test (ELF), FibroTest, TE and SWE in intention-to-treat analysis had excellent diagnostic accuracy and did not differ significantly. Ferraioli et al. (11) recently concluded that this 2D-SWE is accurate for staging LF. Shear wave speed dispersion is highly correlated with LF but not with steatosis. Several guidelines have found that in numerous liver pathologies, the diagnosis of LF with 2D-SWE can replace liver biopsy. The latter is certainly a more invasive test and not without potential complications (11). Overall 2D-SWE gives an advantage to the hepatologist. The latter, in fact, can simultaneously explore the liver parenchyma and perform elastography under direct vision.
The third point is related to the alcoholic competence of hepatologists.
In 2016 we reported the necessity to introduce the hepato-alcohologist (12). This evidence was subsequently demonstrated. ALD should be considered a “dual” disease, as it includes both organ disease and the disease defined as AUD. For this reason, patients should be managed according to an integrated model (addiction team within the internal medicine/hepatology unit). Addolorato argues that integrating AUD interventions with medical management of alcohol-related conditions increases the percentage of patients willing to return for medical checks to manage organ damage and who do not accept a referral solely for addiction treatment (13). It is first necessary to achieve alcohol abstention in order not to compromise medical and surgical hepatological therapy. The relative medical therapy (acute intoxication, withdrawal syndrome, maintenance of sobriety) must be chosen in relation to the severity of the LJ. Addolorato et al. affirm that in patients with ALD persistent alcohol intake is associated with increased mortality while cessation of AC improves survival, medical and surgical treatments for ALD have limited success when drinking continues and the most effective strategy for alcoholics with ALD is to achieve total alcohol abstinence (13). For patient management (especially in the post-LT period) it is necessary to create a support network made up of liver-alcohol service operators, caregivers and self-help mutual associations. It has been evidenced that psychosocial assessment rather than severity of liver failure dominates selection for LT in patients with ALD. In the experience of Daniel et al. (14), Mean Model for End-Stage Liver Disease-sodium scores were similar for selected versus not selected patients with ALD (25 versus 25.6) and selected versus not selected patients with non-ALD (18.3 versus 17.4), although the ALD group had substantially higher Model for End-Stage Liver Disease scores.
Hepato-alcohol services must resolve this frequent problem through close collaboration with informal caregivers or through the reconstruction of a reliable support network. Burden of caregiving for this type of patient is particularly severe. In relation to the constant increase of ALD patients, hepatological and addiction units must partially modify the care organization with the introduction of operators able to manage the training of family members and create a close relationship with the hepatological/addiction service. This can reduce caregiving burden, alcohol relapses, better therapeutic adherence with reduced hospital readmission and social costs. Through education/training, the best knowledge of liver disease (in particular of hepatic encephalopathy), psychiatric pathology and above all alcoholic dependence helps in the care/organizational management of the patient and improves the interpersonal relationship between family members. This is essential when children are present. It is an important aid in restoring reliable family support (15). The latter condition is a fundamental parameter for inclusion in the list for LT. In this club of alcoholics in treatment or other organizations must be supported as they can participate in rebuilding reliable support for ALD patients.
Hepatology patients have changed. They are affected by multiple problems present at the same time (LJ, AUD, hepatic encephalopathy, often psychiatric manifestations, frequent social and family problems). For this reason, the organization of the hepatology units must change. For the hepatologist, it is mandatory to know alcoholology. This type of patient must be managed through a multi-professional activity within the hepatology unit. Furthermore, caregivers and self help associations must be part of the team for optimal management of this complex pathology.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Hepatobiliary Surgery and Nutrition. The article did not undergo external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://hbsn.amegroups.com/article/view/10.21037/hbsn-24-16/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Shroff H, Gallagher H. Multidisciplinary Care of Alcohol-related Liver Disease and Alcohol Use Disorder: A Narrative Review for Hepatology and Addiction Clinicians. Clin Ther 2023;45:1177-88. [Crossref] [PubMed]
- Testino G, Leone S, Borro P. Alcohol and hepatocellular carcinoma: a review and a point of view. World J Gastroenterol 2014;20:15943-54. [Crossref] [PubMed]
- Testino G, Vignoli T, Patussi V, et al. Management of end-stage alcohol-related liver disease and severe acute alcohol-related hepatitis: position paper of the Italian Society on Alcohol (SIA). Dig Liver Dis 2020;52:21-32. [Crossref] [PubMed]
- Parker R, Allison M, Anderson S, et al. Quality standards for the management of alcohol-related liver disease: consensus recommendations from the British Association for the Study of the Liver and British Society of Gastroenterology ARLD special interest group. BMJ Open Gastroenterol 2023;10:e001221. [Crossref] [PubMed]
- Scafato E, Caputo F, Patussi V, et al. The undertreatment of alcohol-related liver diseases among people with alcohol use disorder. Eur Rev Med Pharmacol Sci 2020;24:974-82. [PubMed]
- Testino G, Pellicano R. Panminerva Med 2023;65:391-9. Corrected and republished from: Metabolic associated liver disease. [PubMed]
- European Association for the Study of the Liver. Electronic address: easloffice@easloffice; . EASL Clinical Practice Guidelines: Management of alcohol-related liver disease. J Hepatol 2018;69:154-81. [Crossref]
- Altamirano J, Bataller R, Cardenas A, et al. Predictive factors of abstinence in patients undergoing liver transplantation for alcoholic liver disease. Ann Hepatol 2012;11:213-21. [Crossref] [PubMed]
- Shah ND, Ventura-Cots M, Abraldes JG, et al. Alcohol-Related Liver Disease Is Rarely Detected at Early Stages Compared With Liver Diseases of Other Etiologies Worldwide. Clin Gastroenterol Hepatol 2019;17:2320-2329.e12. [Crossref] [PubMed]
- Thiele M, Madsen BS, Hansen JF, et al. Accuracy of the Enhanced Liver Fibrosis Test vs FibroTest, Elastography, and Indirect Markers in Detection of Advanced Fibrosis in Patients With Alcoholic Liver Disease. Gastroenterology 2018;154:1369-79. [Crossref] [PubMed]
- Ferraioli G, Maiocchi L, Dellafiore C, et al. Performance and cutoffs for liver fibrosis staging of a two-dimensional shear wave elastography technique. Eur J Gastroenterol Hepatol 2021;33:89-95. [Crossref] [PubMed]
- Testino G, Borro P. Alcoholic liver disease and transplantation: the necessity for hepato-alcohologists. Scand J Gastroenterol 2016;51:892. [Crossref] [PubMed]
- Addolorato G, Mirijello A, Barrio P, et al. Treatment of alcohol use disorders in patients with alcoholic liver disease. J Hepatol 2016;65:618-30. [Crossref] [PubMed]
- Daniel KE, Matthews LA, Deiss-Yehiely N, et al. Psychosocial Assessment Rather Than Severity of Liver Failure Dominates Selection for Liver Transplantation in Patients With Alcohol-Related Liver Disease. Liver Transpl 2022;28:936-44. [Crossref] [PubMed]
- Testino G, Bottaro LC, Andorno E, et al. Hepatic encephalopathy: management and diagnostic therapeutic assistance path of Ligurian Local Health Company 3 (ASL3). Minerva Med 2023;114:698-718. [Crossref] [PubMed]


