
Exocrine pancreatic insufficiency: more compromise than precision
Exocrine pancreatic insufficiency (EPI) can be defined as a reduction in the secretion or intraluminal activity of pancreatic enzymes at a level that does not allow the normal digestion of nutrients contained in food. This condition is difficult to diagnose and treat and has long been misunderstood, underestimated, and overlooked to some extent.
However, in the past decades, possibly due to the increasing prevalence of inflammatory and neoplastic pancreatic disorders and awareness that EPI may have serious consequences, this topic has been more extensively considered by health care professionals.
For this reason, we read with great interest the clinical practice updates guidelines on EPI published in Gastroenterology in July 2023 by the American Gastroenterology Association (AGA) in which worldwide recognized experts such as David Whitcomb, Anna Buchner, and Chris Forsmark present best practice advice statements based on available evidence (1).
Notably, during this same timeframe, the United European Gastroenterology (UEG) endorsed a joint initiative of the European Pancreatic Club and other European societies on the same topic, with resulting European guidelines on EPI that are expected to be released before the end of 2024 (2).
AGA guidelines provide useful and pragmatic instructions for clinicians dealing with patients with suspected or confirmed EPI. However, given the lack of high-level evidence, they also serve as a wish list for researchers dealing with pancreatic disorders to prioritize their activity on topics for which many questions remain unanswered or, in the best case, answered by a compromise.
The first issue is the diagnosis of EPI, for which several tests are available, such as direct evaluation of pancreatic secretion through aspiration of pancreatic juice (during secretin-cholecystokinin/cerulein administration), measurement of quantitative fecal fat excretion with calculation of the coefficient of fat absorption, or 13C-mixed triglyceride breath test. However, in real life, the test commonly used in daily clinical practice and recommended by the AGA guidelines as the preferred method for EPI diagnosis is the quantitative measurement of fecal elastase-1 (FE-1). The dosing of FE-1 is a typical example of a compromise that must be made when dealing with EPI. It lies between very expensive, troublesome, and invasive tests, which nonetheless have high diagnostic accuracy, and less expensive and less invasive tests, which frequently fail to diagnose the condition. Thus, FE-1 is necessarily an imperfect test, burdened by a significant number of false positives and false negatives, and must therefore represent only one piece of the puzzle for the diagnosis of EPI, along with symptoms, clinical history, laboratory tests, and imaging studies.
The AGA guidelines support the use of FE-1 in patients with pancreatic conditions and symptoms or signs that may suggest the presence of EPI, and in other subjects in whom EPI is suspected. However, although not in the statements but only in the comments, the document also underlines that in patients with a high pre-test probability of EPI, testing is not necessary as it may result in a significant number of false negatives. We very much agree with this advice.
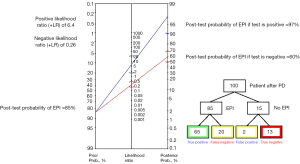
FE-1 has a sensitivity of 88% and a specificity of 88% (3) in a recent meta-analysis. In a pragmatic example, after pancreaticoduodenectomy (PD), the EPI rate is approximately 85%. FE-1 would have a positive likelihood ratio of 6.4 and a negative likelihood ratio of 0.26. Hence, if the test was positive, the post-test probability would increase to 97%, but if it was negative, it would only decrease to 60%. With this performance, for every 100 patients who underwent PD, 20 of the 85 with EPI would be missed by a false negative of FE-1, while 2 of the 15 without EPI would have a false positive result (Figure 1). Therefore, pancreatic enzyme replacement therapy (PERT) should be initiated in all conditions with a high probability of EPI, such as advanced chronic pancreatitis and pancreatic head cancer, and after PD in the presence of symptoms or signs of EPI.
A second important problem is the incorrect use of FE-1 in subjects with a clinical history not suggestive of pancreatic disorders and negative pancreatic imaging. In this scenario, especially in patients with diarrhea, the FE-1 dosage will result in high rates of false positives. Therefore, FE-1 should only be administered to confirm a suspicion arising from clinical history, imaging, and symptoms and signs. This is typically the case in patients with a less advanced stage of chronic pancreatitis or who had acute pancreatitis with tumors in the body/tail of the pancreas, or distal pancreatic resection.
In real life, it is common to receive in pancreatology outpatient clinic patients with intermittent diarrhea, no weight loss, and negative high-resolution pancreatic imaging, who are advised to dose FE-1 that turns out to be low. It is often difficult to convince these individuals that they do not have any pancreatic disorders and do not require PERT. Given the lack of availability of PERT, especially in some countries, inappropriate prescriptions are a very important problem.
Other important issues that remain open in the realm of EPI pertain to clinical management. A crucial point in this regard is how to define the optimal dosing of PERT and evaluate treatment outcomes. PERT, specifically its dosage, represents another compromise in EPI management. The enzyme dosage administered to a patient is purely based on probabilistic and empirical calculations. Theoretically, approximately 90,000 lipase units are secreted during mealtimes. However, as a certain residual enzyme quota remains in most patients (unless they received total pancreatectomy), the AGA guidelines (1), as well as the UEG guidelines for chronic pancreatitis (4), suggest a starting PERT dose of 40,000–50,000 units of enzymes per meal. As FE-1 is not influenced by PERT, it cannot be used to evaluate the treatment response and titrate doses. This is based only on subjective symptomatic improvement reported by the patient and eventually by objective measures of weight loss or nutritional status. However, this assessment may be more complicated than expected. For example, in patients with pancreatic adenocarcinoma, symptoms and malnutrition are multifactorial; thus, understanding whether PERT is sufficient and effective can be challenging. The difficulty and confusion in evaluating the response to PERT is also evident from studies published in the literature, where surrogate outcome measures are often used, such as the frequency of abdominal pain episodes or daily stool frequency, which could be subject to significant biases.
Personalization of PERT has only been attempted in patients with cystic fibrosis, in which user-friendly digital solutions such as mobile applications (apps), taking into consideration the food at each meal, the degree of EPI, and patients’ related variables, are used to advise on the dosage of PERT necessary at each meal (5,6). Another grey area represents the possible indication for PERT in patients with only a mild decrease in FE-1 (between 100 and 200 mg/g). It is debatable whether these patients truly have clinically relevant EPI and thus should be treated with PERT or whether they are in a stage of EPI that could stay without therapy.
Finally, another common issue with this syndrome is its overlap with other diseases that are common in patients with pancreatic disorders and EPI, which can complicate their management and treatment. For instance, small intestinal bacterial overgrowth (SIBO) is common in patients with chronic pancreatitis (7) and after PD (8). Indeed, pancreatic juice has antimicrobial activity, which is impaired in patients with EPI (9). Therefore, while AGA mentions SIBO among the possible differential diagnoses in patients with EPI, it should be considered as a possible complication in these patients and should be actively sought and treated, especially when the response to PERT is suboptimal.
In conclusion, the current practical recommendations issued by the AGA on EPI are very important but are mostly based on expert opinions and observational studies with limited evidence. There is a need for further high-quality scientific evidence to reduce compromises and to employ precision medicine in the diagnosis and treatment of EPI.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Hepatobiliary Surgery and Nutrition. The article did not undergo external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://hbsn.amegroups.com/article/view/10.21037/hbsn-24-92/coif). P.G.A. reports honoraria for lectures from Boston Scientific, Olympus, Cook Medical and Pentax and is on Steering committee of AMBU and Mediglobe. G.C. reports grant from AIRC (Associazione Italiana Ricerca sul Cancro), consulting fees from Viatris, Boston Scientific and Pangenix. The other author has no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Whitcomb DC, Buchner AM, Forsmark CE. AGA Clinical Practice Update on the Epidemiology, Evaluation, and Management of Exocrine Pancreatic Insufficiency: Expert Review. Gastroenterology 2023;165:1292-301. [Crossref] [PubMed]
- PEI Guidelines | European Pancreatic Club. Available online: https://www.europeanpancreaticclub.org/about-us/diagnosis-and-treatment-guidelines/european-guidelines-on-the-diagnosis-and-therapy-of-pancreatic-exocrine-insufficiency-pei/
- Vanga RR, Tansel A, Sidiq S, et al. Diagnostic Performance of Measurement of Fecal Elastase-1 in Detection of Exocrine Pancreatic Insufficiency: Systematic Review and Meta-analysis. Clin Gastroenterol Hepatol 2018;16:1220-1228.e4. [Crossref] [PubMed]
- Löhr JM, Dominguez-Munoz E, Rosendahl J, et al. United European Gastroenterology evidence-based guidelines for the diagnosis and therapy of chronic pancreatitis (HaPanEU). United European Gastroenterol J 2017;5:153-99. [Crossref] [PubMed]
- Boon M, Calvo-Lerma J, Claes I, et al. Use of a mobile application for self-management of pancreatic enzyme replacement therapy is associated with improved gastro-intestinal related quality of life in children with Cystic Fibrosis. J Cyst Fibros 2020;19:562-8. [Crossref] [PubMed]
- Calvo-Lerma J, Hulst J, Boon M, et al. Clinical validation of an evidence-based method to adjust Pancreatic Enzyme Replacement Therapy through a prospective interventional study in paediatric patients with Cystic Fibrosis. PLoS One 2019;14:e0213216. [Crossref] [PubMed]
- Capurso G, Signoretti M, Archibugi L, et al. Systematic review and meta-analysis: Small intestinal bacterial overgrowth in chronic pancreatitis. United European Gastroenterol J 2016;4:697-705. [Crossref] [PubMed]
- Muniz CK, dos Santos JS, Pfrimer K, et al. Nutritional status, fecal elastase-1, and 13C-labeled mixed triglyceride breath test in the long-term after pancreaticoduodenectomy. Pancreas 2014;43:445-50. [Crossref] [PubMed]
- Minelli EB, Benini A, Bassi C, et al. Antimicrobial activity of human pancreatic juice and its interaction with antibiotics. Antimicrob Agents Chemother 1996;40:2099-105. [Crossref] [PubMed]


