
Mortality from liver cirrhosis and HCC in the DAA era: success in viral control is darkened by raise of metabolic disease
Liver cirrhosis and primary liver cancers are leading causes of mortality worldwide with over than 1.7 million of deaths in 2010 representing about 3.4% of the overall deaths (1). Global liver cirrhosis deaths ceaselessly increased by 52.2% from 1980 to 2010 (1). Similarly, primary liver cancers global deaths increased by 62.4% from 1990 to 2010 (2). Chronic viral (i.e., HBV and HCV), alcoholic (ALD) and non-alcoholic fatty liver (NAFLD) diseases are the most important etiologies of liver cirrhosis and hepatocellular carcinoma (HCC). In the last years, the introduction of direct antiviral agents (DAAs) has revolutionized HCV care. Indeed, DAAs are highly effective (cure rates higher than 90%) and well tolerated even by difficult-to-treat candidates as patients with advanced liver cirrhosis. However, the global impact of these progresses on advanced liver disease and HCC remains to be determined. While viral cure has been shown to decrease the overall HCC risk in HCV-infected patients, accumulating clinical evidences in large cohort studies demonstrate that HCC risk persists after HCV cure especially in advanced fibrosis (3,4) with an annual HCC incidence between 1–12% per year. Furthermore, an unexpected high rate of early HCC recurrence following DAA treatment in some studies but not in others has raised concerns on the effect of these drugs in HCC prevention (5). Finally, a large majority of HCV-infected patients has no access to DAAs due to high costs.
Highly effective and tolerate antiviral agents for treatment of chronic hepatitis B were also introduced in clinical practice in the last 15 years. Indeed, entecavir was FDA-approved in 2005 and tenofovir disoproxil fumarate in 2008. While antiviral drugs have been shown to prevent or reverse hepatic decompensation and to reduce the prevalence of virus-induced end-stage liver disease (6,7), data on their effect on mortality on a population level are largely lacking.
At the same time, the incidence of NAFLD-related chronic liver failure and HCC has increased dramatically and ALD has been reported as the most common cause of chronic liver disease (7,8). Data from United Network for Organ Sharing (UNOS) cohort revealed a significant decrease in the prevalence of HCV and an increase of NAFLD or ALD among patients new to the liver transplant waitlist or undergoing liver transplantation for liver cirrhosis (7). However, among patients transplanted for HCC, the proportions of HCV infection, NAFLD and ALD did not change between 2003 and 2015 (7).
To better understand the epidemiological changes in the etiologies of advanced liver disease and evaluate the impact of the novel antiviral treatments on a population level, updated incidence and mortality data of the last decade are essentially needed.
In the article by Kim et al. recently published in Hepatology (9), the authors performed an elegant analysis of the mortality trends for liver cirrhosis and HCC in the United States over the last 10 years in adults aged ≥20 years. Using mortality records from the Centers for Disease Control and Prevention’s National Vital Statics System that uses the International Classification of Disease, Tenth Revision (ICD-10) to codify diseases, they calculated age-specific mortality rates and used joinpoint regression to determine the annual percentage change (APC) of mortality for both cirrhosis and HCC. APCs of mortality rates according to the major etiologies, ethnicities and sex were also assessed.
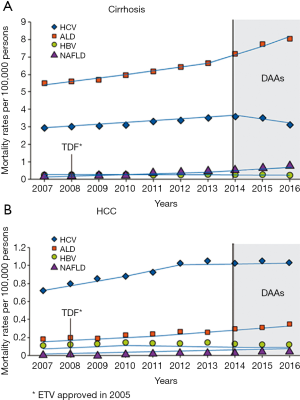
The authors found that in U.S. the age-standardized cirrhosis-related mortality rates increased from 19.77/100,000 persons in 2007 to 23.67 in 2016 with an average annual increase of 2.3%, and similarly, HCC-related mortality increased from 3.48 persons in 2007 to 4.41 in 2016 at an annual rate of 2.0% (9).
Interestingly, the APC of HCV-related cirrhosis mortality shifted from an increase of 2.9% per year during 2007–2014 to a reduction of 6.5% per year during 2014–2016. In parallel, mortality for ALD-related and NAFLD-related cirrhosis increased over the study period with an APC of, respectively, 4.5% and 15.4% per year. Inversely, mortality for HBV-related cirrhosis decreased with an average APC of −1.1% (9).
Regarding HCC, age-standardized mortality rates in U.S. for HCV-related HCC increased (APC 7.0%) and reached a plateau in 2012 remaining stable from 2012 to 2016 (APC 0.4%). A linear increase in the age-standardized HCC-related mortality rates for ALD and NAFLD was observed from 2007 to 2016 (APC respectively 7.4% and 19.1%). Concerning HBV, a trend in increased HCC mortality (APC +6.3%) was observed between 2007 and 2010 while an inverse trend (−2.2%) was noted in the period 2010–2016 (9).
Here, Kim et al. showed that since the introduction of DAAs in U.S. in late 2013, there has been a significant decrease in HCV-related cirrhosis mortality rates compared with the pre-DAA era. Importantly—since an alert on the association between DAAs and early HCC recurrence was raised in 2016 (10,11)—no increase in HCV-related HCC mortality after the DAA introduction was observed. It is of interest to note that HCC is a late event in the natural history of chronic liver diseases. Long-term follow-up studies have observed that 1–8% of patients with cirrhosis develop HCC per year (3,12). This implies that long-term studies (>10 years) are needed to evaluate any benefit of antiviral treatments on HCC mortality. Kim et al. showed that HCV-related HCC mortality did not raise after 2012 and that HBV-related HCC mortality started to steadily decrease after 2010.
Other relevant findings of this study are the data on ALD and NAFLD. The mortality rates for ALD and NAFLD dramatically increased during the 10-year study period. In 2016, among patients with cirrhosis, ALD had the highest age-standardized mortality rate, more than the double of HCV (8.23/100,000 persons vs. 3.20) with an APC of +4.5%. At the same time, NAFLD is the third cause of cirrhosis mortality (0.82/100,000 persons in 2016) and the fourth cause of HCC mortality (0.06/100,000 persons in 2016) with impressive APCs of respectively +15.4% and +19.1%. These trends could be partly explained by the increased awareness and improvement in diagnosis in the last 10 years even though the ICD coding system has shown to underestimate NAFLD prevalence and mortality. However, it is important to note that in spite of the ALD and NAFLD trends, HCV still accounted for most of HCC deaths during the study period confirming the different cancer risk between viral and metabolic diseases (12).
Several U.S. studies also demonstrated that, in the last 15 years, inpatient mortality from liver cirrhosis significantly declined over time (13,14). Then, the trends in cirrhosis mortality presented by Kim et al. confirms that some burden of mortality cirrhosis shifted from the in-hospital to the outpatient setting as already suggested by previous Veterans Administration hospitals’ data (14).
Finally, a subgroup analysis of mortality by ethnical groups was conducted. In 2016, non-Hispanic whites and Hispanic had the highest age-standardize cirrhosis mortality while non-Hispanic blacks and non-Hispanic Asian had the highest HCC mortality. In terms of APC, non-Hispanic whites had the highest APC in cirrhosis and HCC-related mortality (respectively +3.5% and +2.4% per year) while non-Hispanic Asians were the only ethnic group showing a significant APC reduction in HCC mortality with a decline of 3.5% per year. The interpretation of these data is difficult because no adjustment for etiology’s prevalence, income and/or access to care was performed. A recent study showed that a significant variability exists in U.S. in liver disease-related mortality among states and is independent from the prevalence of alcohol consumption and obesity while strongly correlates with high prevalence of Hispanic individuals, viral hepatitis and low income (15).
In conclusion, the work by Kim et al. provides the liver community with relevant data about the changes in cirrhosis and HCC mortality in U.S. over the last 10 years (Figure 1). In the DAA era, HCV-cirrhosis mortality significantly decreased while HCV-HCC mortality did not increase after 2012. After the introduction of high-barrier nucleoside and nucleotide analogues for HBV, HBV-cirrhosis mortality has constantly decreased. Studies with longer follow-up are needed to capture changes in the mortality of HBV and HCV-related HCC. Concurrently, mortality rates for ALD and NAFLD associated cirrhosis and HCC dramatically increased in the last years. Public policies and treatment strategies are urgently required to further reduce liver disease mortality with a special focus on metabolic liver disease.
Acknowledgments
Funding: This work was supported by Inserm, the University of Strasbourg, the European Union (Infect-ERA hepBccc, ERC-2014-AdG-671231-HEPCIR and Horizon 2020 research and innovation programme under grant agreement 667273 - HEPCAR), the Agence Nationale de Recherches sur le Sida et les Hépatites Virales (ANRS 15/1099), the French Cancer Agency (ARC IHU201301187) and the US National Institutes of Health (NIH/NIAID U19 AI123862-01, NIH/NIAID R03 AI131066, NIH/NCI R21 CA209940). This work has been published under the framework of the LabEx ANR-10-LAB-28 and benefits from a funding from the state managed by the French National Research Agency as part of the Investments for the Future (Investissements d’Avenir) program. A.S. is the recipient of a fellowship co-funded by the Région Alsace, France, the LabEx HepSys and IHU Strasbourg.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Mokdad AA, Lopez AD, Shahraz S, et al. Liver cirrhosis mortality in 187 countries between 1980 and 2010: a systematic analysis. BMC Med 2014;12:145. [Crossref] [PubMed]
- Lozano R, Naghavi M, Foreman K, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2095-128. [Crossref] [PubMed]
- Kanwal F, Kramer J, Asch SM, et al. Risk of Hepatocellular Cancer in HCV Patients Treated With Direct-Acting Antiviral Agents. Gastroenterology 2017;153:996-1005.e1. [Crossref] [PubMed]
- van der Meer AJ, Feld JJ, Hofer H, et al. Risk of cirrhosis-related complications in patients with advanced fibrosis following hepatitis C virus eradication. J Hepatol 2017;66:485-93. [Crossref] [PubMed]
- Llovet JM, Villanueva A. Liver cancer: Effect of HCV clearance with direct-acting antiviral agents on HCC. Nat Rev Gastroenterol Hepatol 2016;13:561-2. [Crossref] [PubMed]
- Lim YS, Han S, Heo NY, et al. Mortality, liver transplantation, and hepatocellular carcinoma among patients with chronic hepatitis B treated with entecavir vs lamivudine. Gastroenterology 2014;147:152-61. [Crossref] [PubMed]
- Goldberg D, Ditah IC, Saeian K, et al. Changes in the Prevalence of Hepatitis C Virus Infection, Nonalcoholic Steatohepatitis, and Alcoholic Liver Disease Among Patients With Cirrhosis or Liver Failure on the Waitlist for Liver Transplantation. Gastroenterology 2017;152:1090-9.e1. [Crossref] [PubMed]
- Beste LA, Leipertz SL, Green PK, et al. Trends in burden of cirrhosis and hepatocellular carcinoma by underlying liver disease in US veterans, 2001-2013. Gastroenterology 2015;149:1471-82.e5; quiz e17-8.
- Kim D, Li AA, Perumpail BJ, et al. Changing Trends in Etiology- and Ethnicity-Based Annual Mortality Rates of Cirrhosis and Hepatocellular Carcinoma in the United States. Hepatology 2019;69:1064-74. [Crossref] [PubMed]
- Conti F, Buonfiglioli F, Scuteri A, et al. Early occurrence and recurrence of hepatocellular carcinoma in HCV-related cirrhosis treated with direct-acting antivirals. J Hepatol 2016;65:727-33. [Crossref] [PubMed]
- Reig M, Mariño Z, Perelló C, et al. Unexpected high rate of early tumor recurrence in patients with HCV-related HCC undergoing interferon-free therapy. J Hepatol 2016;65:719-26. [Crossref] [PubMed]
- Ioannou GN, Green P, Lowy E, et al. Differences in hepatocellular carcinoma risk, predictors and trends over time according to etiology of cirrhosis. PLoS One 2018;13:e0204412. [Crossref] [PubMed]
- Schmidt ML, Barritt AS, Orman ES, et al. Decreasing mortality among patients hospitalized with cirrhosis in the United States from 2002 through 2010. Gastroenterology 2015;148:967-77.e2. [Crossref] [PubMed]
- Kanwal F, Tansel A, Kramer JR, et al. Trends in 30-Day and 1-Year Mortality Among Patients Hospitalized With Cirrhosis From 2004 to 2013. Am J Gastroenterol 2017;112:1287-97. [Crossref] [PubMed]
- Desai AP, Mohan P, Roubal AM, et al. Geographic Variability in Liver Disease-Related Mortality Rates in the United States. Am J Med 2018;131:728-34. [Crossref] [PubMed]


