
Prevent bile duct injury by indocyanine green guide fluorescent imaging during laparoscopic cholecystectomy in liver transplantation recipient
Cholecystolithiasis with acute cholecystitis is a rare, late biliary complication occurring in liver transplantation (LT) recipients who received the liver graft with preserved donor’s gallbladder. Although laparoscopic cholecystectomy (LC) is not contraindicated after upper abdominal surgery, misunderstanding of the biliary anatomy due to inflammatory phenomena or severe adhesion might increase the risk of bile duct injury (BDI) (1).
Herein we presented a case of 40-year-old male patient who underwent orthotopic liver transplantation (OLT) on 2006 due to hepatitis B virus related acute on chronic liver failure. The liver graft weighted 1,864 gm and gallbladder was preserved. Allograft cholecystostomy with Foley catheter was performed during operation. 13 years later, he suffered from acute cholecystitis with sepsis and biliary subcutaneous fistula. Antibiotics followed by percutaneous transhepatic gallbladder drainage (PTGBD) was performed as initial treatment. The patient was scheduled for LC 8 months after PTGBD after acute inflammation completely subsided.
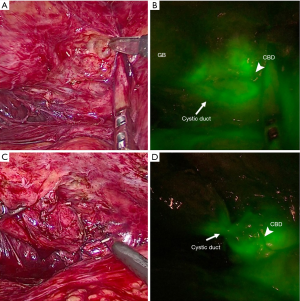
During the LC, near-infrared (NIR) cholecystocholangiography with direct intra-gallbladder indocyanine green (ICG) injection method was applied. According to our previous experience (2), we inject 10 mL bolus of ICG (DiagnoGreen, Taiwan, ROC) at a concentration of 0.125 mg/mL from PTGBD to achieve best visualization of entire biliary anatomy. Gr IV adhesion due to previous operation and severe inflammation status was found. Under the guide of ICG fluorescent imaging, we were able to identify the cystic duct and common bile duct junction clearly, which is not visible under white light (Figure 1A,B). The dissection and ligation of cystic artery and cystic duct was performed under the guidance of ICG fluorescent imaging (Figure 1C,D). Total operation time was 240 minutes and estimated blood loss was 100 mL. The patient was discharged on postoperative day 9 without any surgical complication.
Biliary complications remain a common problem after LT, which are associated with significant morbidity and mortality (2–7%), retransplantations (6–12.5%) and one of the leading causes of graft dysfunction or loss (3). In the very early era of OLT, gallbladder was preserved as a conduit between the donor and the recipient bile ducts for biliary tract reconstruction in order to perform procedure to treat post-transplant biliary complications (4). The technique has been abandoned due to increasing episode of cholangitis and bile stasis with stones formation, which may result in inferior outcome to LT patients (5). Although our center had no more preserved gallbladder in OLT for more than 10 years, the late complication such as cholecystolithiasis and acute cholecystitis remain the critical problem to LT patients, which had been reported to occur 14–19 years after OLT (6).
Conventionally, intraoperative cholangiography (IOC) had been use to map biliary anatomy and enhance the safety of LC. However, the routine use of IOC is controversial due to time consuming, radiation exposure and the need for additional equipment and trained personnel (7). Our technique of NIR cholecystocholangiography with ICG fluorescent imaging provides a rapid and noise-free visualization of biliary anatomy. Notably, we encountered grade IV adhesion with large part of the bowel adhesion to liver hilar and gallbladder. With the guide of NIR cholecystocholangiography with ICG, we are able to identify the biliary anatomy during our enterolysis and performed dissection without unnecessary BDI.
In conclusion, our technique could be used in patients with inflammatory and adhesion status after abdominal surgery such as LT, and it could also enhance the safety and minimize BDI by mapping biliary anatomy real-timely during LC.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article is a free submission to the editorial office, Hepatobiliary Surgery and Nutrition. The article has been sent for external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://hbsn.amegroups.org/article/view/10.21037/hbsn-20-342/coif). CLC serves as an unpaid editorial board member of Hepatobiliary Surgery and Nutrition. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Machado NO. Biliary complications postlaparoscopic cholecystectomy: mechanism, preventive measures, and approach to management: a review. Diagn Ther Endosc 2011;2011:967017. [Crossref] [PubMed]
- Liu YY, Liao CH, Diana M, et al. Near-infrared cholecystocholangiography with direct intragallbladder indocyanine green injection: preliminary clinical results. Surg Endosc 2018;32:1506-14. [Crossref] [PubMed]
- Londoño MC, Balderramo D, Cárdenas A. Management of biliary complications after orthotopic liver transplantation: the role of endoscopy. World J Gastroenterol 2008;14:493-7. [Crossref] [PubMed]
- Yanaga K, Sugimachi K. Biliary tract reconstruction in liver transplantation. Surg Today 1992;22:493-500. [Crossref] [PubMed]
- Anselmi M, Sherlock D, Buist L, et al. Gallbladder conduit vs end-to-end anastomosis of the common bile duct in orthotopic liver transplantation. Transplant Proc 1990;22:2295-6. [PubMed]
- Vernadakis S, Sotiropoulos GC, Fouzas I, et al. Cholecystectomy due to symptomatic gallbladder disease after orthotopic liver transplantation: report of three cases. Transplant Proc 2012;44:2757-8. [Crossref] [PubMed]
- Khan OA, Balaji S, Branagan G, et al. Randomized clinical trial of routine on-table cholangiography during laparoscopic cholecystectomy. Br J Surg 2011;98:362-7. [Crossref] [PubMed]


