Markedly elevated liver transaminases following pancreaticoduodenectomy: celiac artery thrombosis in disguise
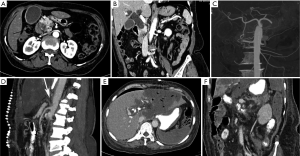
A 63-year-old lady underwent classical pancreaticoduodenectomy with regional lymphadenectomy for periampullary cancer. Preoperative contrast-enhanced computed tomography (CECT) of abdomen revealed dilated common bile duct which showed abrupt cut-off at ampulla. CECT also revealed replaced right hepatic artery arising from the left gastric artery (Panels A-C). During surgery, gastroduodenal artery was test-clamped to confirm pulsations in the hepatic artery before being ligated. On third postoperative day, she was found to have altered sensorium. Liver function tests showed bilirubin of 10.9 mg%; however, liver transaminases were markedly elevated (AST of 2,095 U/L and ALT of 1,243 U/L)—prothrombin time was also elevated [international normalized ratio (INR) =2.2]. Postoperative CECT of abdomen and pelvis revealed thrombosis of celiac artery trunk resulting in marked liver and spleen necrosis. Distal right hepatic artery was reformed by the collaterals; it explains relative sparing of right lobe of liver (Panels D-F).
Marked elevation of liver transaminases suggesting acute hepatic insult is a rare immediate postoperative complication following pancreaticoduodenectomy; however, if present, this may be caused by drug induced hepatotoxicity, blood transfusion reaction, co-existent viral hepatitis, sepsis or perioperative hypotension. The etiological factors for celiac artery thrombosis are arteriosclerosis, hyper-coagulable states, extrinsic stenosis (celiac artery stenosis—compression by median arcuate ligament, the celiac ganglia or surrounding local fibro-inflammatory tissue), cancer, surgical trauma, congenital stenosis, catheter related injury during endovascular therapy, and idiopathic. Presence of celiac artery stenosis is not-so-uncommon entity; pancreatic surgeons must be aware of this vascular entity to avoid potentially catastrophic ischemic complications after pancreaticoduodenectomy.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Informed consent was obtained from the patient for publication of this article and any accompanying images.