Spontaneous bilateral adrenal hemorrhage following cholecystectomy
A 45-year-old obese woman underwent an uncomplicated laparoscopic cholecystectomy for acute cholecystitis. Because of past history of a deep lower limb venous thrombosis during pregnancy, she was under prophylactic low-molecular-weight heparin during the perioperative period. The postoperative course was uneventful and she was discharged on postoperative day 7, only because of wound infection. On postoperative day 9, the patient was readmitted to our department for abdominal pain, fever, nausea and vomiting. Physical examination showed diffuse abdominal pain and tenderness. There was no guarding or rebound and her wounds were healing normally. Laboratory results showed the following: white blood cell count 17×109/L, hemoglobin 10.4 g/dL, platelet count 850×109/L, natremia 132 mmol/L, and kaliema 4.9 mmol/L. Liver tests were within the normal range and prothrombin time was more than 80%.
Computed tomography and magnetic resonance imaging revealed bilateral adrenal hemorrhage (Figure 1). Laboratory results revealed a low serum cortisol of 54 nmol/L (normal values between 171 and 536 nmol/L). The antiphospholipid antibodies revealed the presence of significant lupus anticoagulant. A diagnosis of bilateral adrenal hemorrhage associated with primary adrenal insufficiency was made.
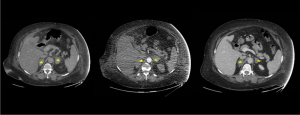
Postoperative adrenal hemorrhage is a rare but potentially life-threatening complication if the condition is bilateral with a risk of adrenal failure. This diagnosis of often missed because the symptoms and laboratory results are usually nonspecific. Bilateral adrenal hemorrhages have been mostly described to be associated with heparin-induced thrombocytopenia (1), antiphospholipid syndrome (2) and sepsis (3). The diagnosis of adrenal hemorrhage can be made by a computed tomography showing adrenal gland enlargement with high attenuation without contrast enhancement. Our patient was treated with fludrocortisone treatment and curative anticoagulation. She’s going well 6 months after.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the editor-in-chief of this journal.
References
- Ramon I, Mathian A, Bachelot A, et al. Primary adrenal insufficiency due to bilateral adrenal hemorrhage-adrenal infarction in the antiphospholipid syndrome: long-term outcome of 16 patients. J Clin Endocrinol Metab 2013;98:3179-89. [Crossref] [PubMed]
- Warkentin TE, Sayfan EL, Linkins LA. Heparin-induced thrombocytopenia presenting as bilateral adrenal hemorrhages. N Engl J Med 2015;372:492-4. [Crossref] [PubMed]
- Hiroi N, Ishimori H, Kaneko Y, et al. Bilateral adrenal hemorrhage due to sepsis resulting in acute adrenal crisis. Intern Med 2005;44:1017-8. [Crossref] [PubMed]


